Solutions > Medicaid
mPulse for Medicaid
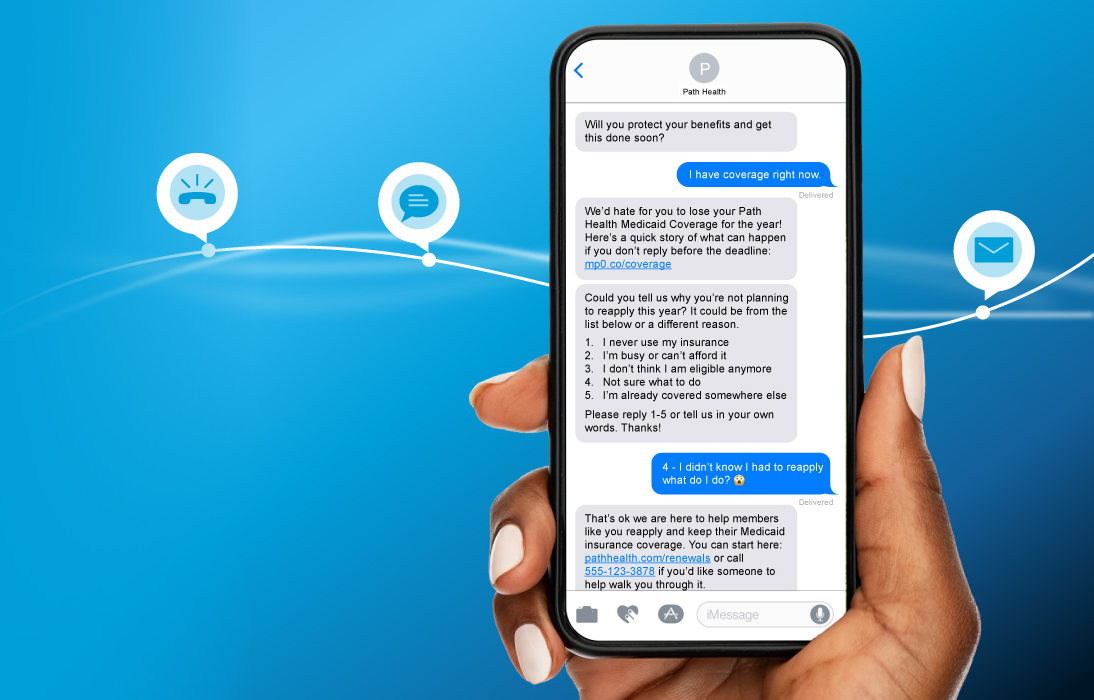
Leading Medicaid plans work with mPulse to deliver highly tailored, meaningful interactions that inspire behavior change and groundbreaking outcomes.
Highly Personalized to Each Member
Plan for the unwinding of continuous enrollment and the reentrance of redetermination
Addressing The Needs of Medicaid Plan Members

Conversational AI Across Languages
Deliver meaningful / sophisticated / best-in-class outreach to non-English speaking members.
Health Literacy Focus
Build health skills and understanding through captivating digital content.
SDoH Barriers
Use conversational outreach to uncover and address the areas where individuals need support.
We Solve Medicaid’s Most Important Challenges
mPulse’s knowledge of Medicaid member diversity and lifestyle preferences enables us to deliver the right touchpoints through the right channel at key moments throughout each member’s unique journey.
Prevention & Screenings
Customer:
Leading health plan in NV
Objective:
Encourage unengaged members to close related HEDIS care gaps
Results:
43% gap closure improvement across 11 measures compared to control group
Customer:
Mid-Atlantic MCO
Objective:
Reduce Medicaid churn by switching from direct mail to SMS
Results:
9pp reduction in churn with prior-express consent SMS messaging enabling 289% greater reach
Customer:
Leading plan in IN
Objective:
Educate members about alternative care options to reduce ER overutilization
Results:
69.7% reduction in ER visists among 11,668 high utilizers
Don’t take our word for it
Leading Medicaid Plans trust mPulse
LATEST NEWS & RESOURCES
Are You Ready?
health outcomes through market leading health engagement solutions.