During the RISE West conference earlier this month, there were a lot of conversations about the changes that face healthcare in the new year. 2020 brought on a lot of changes to CAHPS measures and weighting that will not only affect the new year, but transform the way Medicare plans will be evaluated and rewarded for the foreseeable future. mPulse Mobile focused on 4 strategies to prepare for 4X CAHPS ratings during our roundtable at RISE West, and it fell in line with what the conference presented overall. Here are our takeaways from the event both the roundtable and the conference.
Focus on Creating a Relationship
Plans will need to keep up with the changing quality guidelines, including the change of CAHPs survey scores to 4x weighting. Everyone knows running a successful Stars program has always been more of a marathon than a sprint. Plans do everything they can to improve member experience and health outcomes on a daily basis, year over year, in an effort to maintain and attain high performing status. It comes as no surprise, COVID 19 has thrown a wrench in those plans and now the marathon has become a decathlon – hurdles around each corner, new sprints to the finish, jumping over and through an ever changing regulatory landscape while throwing everything you have left at anything you can hit.
What’s interesting about these changes are how plans will have less focus on traditional priorities as they are weighted differently. The opportunity here is to think beyond traditional HEDIS and medication adherence improvement strategies and deploy solutions that will engage members in a way that builds a rapport between member and plan or provider.
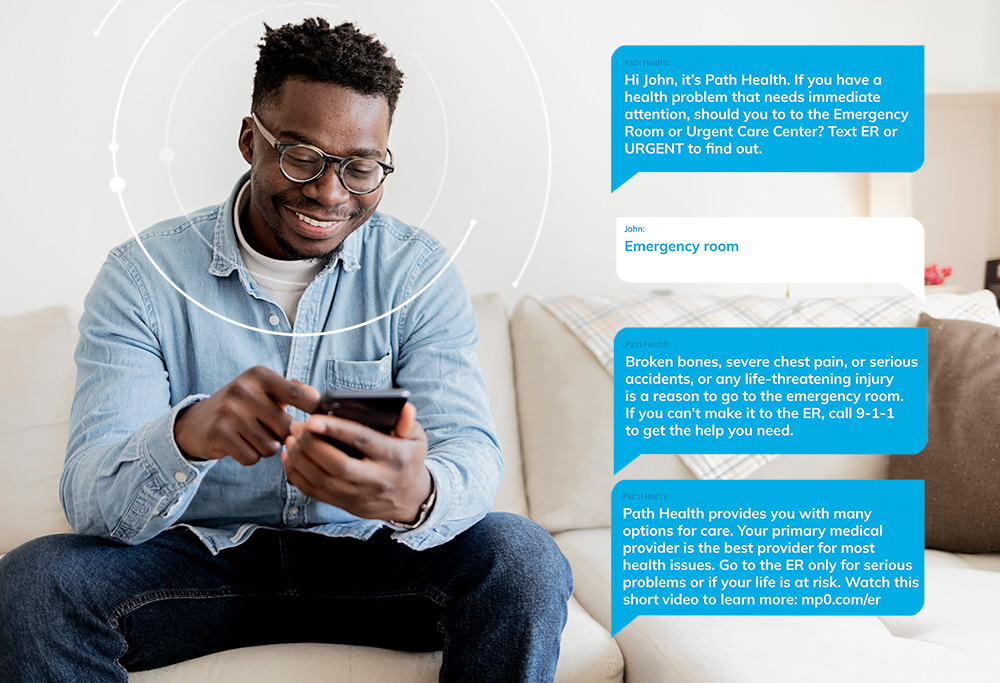
Creating new touchpoints with members where they can respond and feel heard is critical. mPulse uses automated “check-in’s” and follow ups after customer service interactions to create scalable conversations with members. By listening to member responses and answering back, we both gather key data and give members a chance to have 2-way interaction with their plan on their terms.
In the roundtable, we noted that all of those best laid plans for 2021 Stars don’t have to fail or be seen as all for naught. Even though CMS has recycled last year’s CAHPS and HEDIS rates for 2021 Stars, the hard work and efforts put in over the last few years are likely still improving member experience and health outcomes, it just won’t be displayed as such on Medicare Plan Finder.
Be Proactive
Engaging members about their experience with their plan via automated message helps gather necessary data to respond to the member, but also provides an opportunity and touchpoint to share good news about plan changes. Sharing new information that may affect the way the member interacts with their plan will build trust and help further establish that onboarding process that will lay the groundwork for future conversations. A proactive approach around potentially negative news or changes helps eliminate surprises for members who may not be otherwise aware of a formulary change until they get to a pharmacy.
Act on the Experience Data You Have
2021’s changes require MA plans to listen to what members are saying more than ever before: the good, the bad, and the in-between. Taking stock of every member touchpoint and the data it generates is key to tailoring communication with the member. And while plans usually think of experience information as call center or appeal/grievance data, virtually any information the plan has can be used to create a meaningful interaction or make an existing one more impactful. Just member date of birth and date of joining the plan create opportunities for birthday reminders, health plan anniversaries, or milestones and shows that the plan is interested in the member. mPulse takes member responses to surveys or automated outreach and applies sentiment and intent analysis. This takes a strong initial data point and enriches it so that the plan can see, for instance, how members respond to gaps in care outreach, as well as those who are consistently negative or positive in their interactions with the plan. And by building personas around trends in experience data, plans can better predict “look-alikes” who may be more likely to have a neutral or negative opinion of the plan but have not filed a grievance or complaint.
Understand the Member Experience Impact of Telehealth
Plans can implement CAHPS improvement strategies and customer service operations to optimize member experience around digital care. The last six months have essentially forced beneficiaries, carriers, and providers to embrace innovations and technology. Now there is a need to improve member experience with digital and remote care and how its value is communicated to members. Plans who engage and support their membership through this new and ever evolving space will come out on top. It takes more than just letting a member know they have coverage for telehealth visits, it takes an extra effort to educate and encourage them. Creating interactions where members can share barriers, hesitations or concerns with telehealth will be key to an effective CAHPS strategy in 2021.
Plan for a Second Wave of COVID-19 and Strategies to Close Gaps in the Meantime
It is difficult to predict the lingering impact of COVID-19 in late 2020 and early next year. However, when plans begin to shift towards post-COVID strategies, they will need to remain agile and ready to accommodate shifts in public health guidance and CMS rules. In general, plans should not wait to encourage members to complete key preventive care visits and screenings if possible and stay adherent with medications. Knowing that more changes from CMS are coming, plans should continue both maximizing their performance now, and putting processes in place to be successful when Stars returns to “normal” and COVID-19 rule changes no longer protect ratings.
Plans who make an effort to build stronger connections with members and execute a deeper CAHPS strategy now will be more likely to see a successful Stars season in 2022. Since better relationships with members do not necessarily reset every measurement year, it’s also the area where plans can see the most value for their quality improvement efforts now.