mPulse Mobile is a leader in conversational AI solutions for the healthcare industry. We work with 100+ healthcare partners and have deployed over 300 million messages to healthcare members. mPulse’s CTO, Ram Prayaga, sat down with VP of Marketing, Brendan McClure at AHIP’s Consumer Experience & Digital Health Forum 2020 last week to discuss how we execute Conversational Member Engagement: Data, Experience, and Outcomes. Here are our key takeaways:
Orchestration of AI Conversational Engagement
At any given time, plans have multiple departments that are prioritizing topics of interest for their members, so how does a plan coordinate those touchpoints and maintain a relevant member-centric strategy? The answer is data. Plans that utilize the data collected from conversations and interactions with their members and leverage tools that incorporate that data to tailor content and frequency will be more successful at reaching large populations with an approach that meets each plan and member needs. While it may be difficult to curate messaging for each member, with an omnichannel and AI-enabled system, plans are able to implement tailored content and promote a more coordinated outreach cadence for each member or population segment.
How do Plans Gather Conversational Engagement Data?
Although conversational data is a newer type of data, it has become a valuable tool when reaching out to members at scale. Brendan mentioned in the session that insights from conversational outreach can be used in a number of ways to “Give the plan an important read on experience.” A plan can analyze member responses to understand sentiment and intent, as well as see how members navigate through interactive programs to identify opportunities to optimize future outreach. Ram guided the audience through primary touchpoints that conversational engagement data impacts in the member experience. He talked through mPulse’s barriers assessment, which allows a plan to learn the why behind a member may not be meeting their health goal and the plan’s target outcome. He talked about mPulse’s analysis of sentiment and intent of member responses, which can scale from positive to neutral to negative, which gives a plan more data to tailor messaging and meet preferences. All of this information is gathered by engaging in a natural dialogue via interactive messaging – such as text messages – versus deploying a full off-cycle CAHPS survey, for example. The plan can also glean this experience data needed from conversations, rather than relying on survey questions asking the member for it directly.
How Can Plans Engage at Scale?
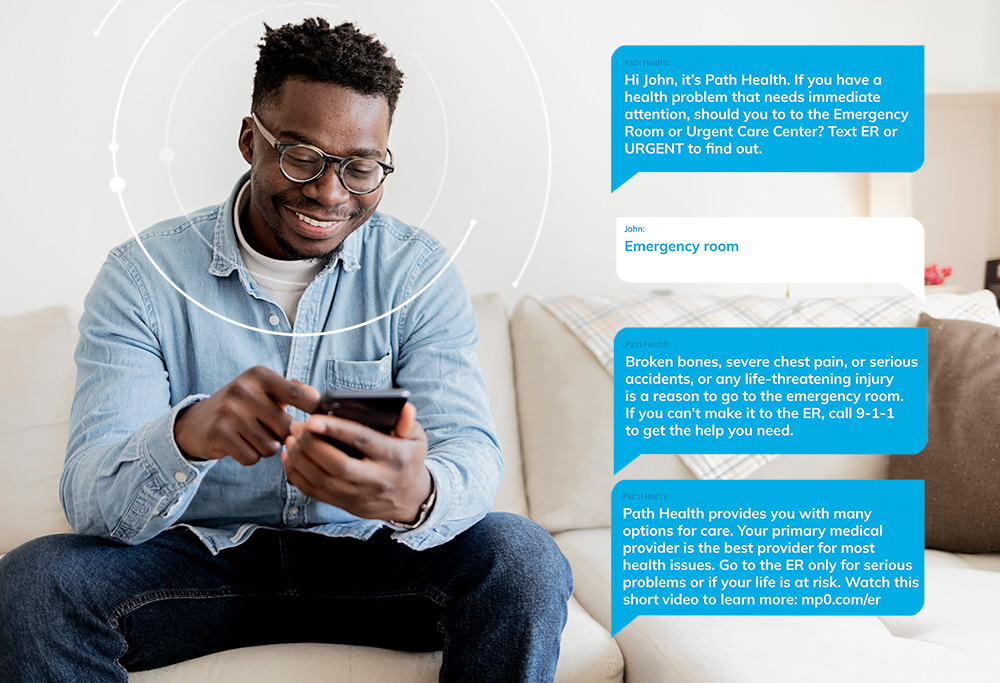
Utilizing artificial intelligence in text conversation allows plans to deploy messages to millions of members with a more natural, conversational experience. In order to maintain a good connection with thousands of people at the same time, plans need to understand what people are saying, measure it and store that information for future touchpoints. Conversational AI, integrated with an omnichannel approach, is the perfect tool for that goal. Most members have access to a mobile phone and text regularly, including senior populations, but for the members who are most engaged through IVR, mailers, and other alternative routes of communication, plans will still need to consider meeting their members where they are. Adding an automated conversational solution can help support a multi-pronged communication approach to reach members in the channels they prefer with impactful dialogue.
How Do you Maintain the Human Touch?
The best engagement feels natural and easy for members. A simple act like listening to the members preference on the best time of day to initiate a conversation, or starting the conversation with content that is relevant to the individual will make a difference in the members response. How a plan manages members preferences is vital. When thinking about member-centric outreach, a plan can look at different ways to engage a member in a dialogue that listens versus putting them on a one way automated track. When we think about human conversations, we do not converse in a linear manner. Often times the conversation will jump from one topic to the other in a short period of time. A truly conversational solution should be able to listen to those pivots in the dialogue and accommodate its workflow to respond with relevant information that follows along with what the member is saying in real time. This means having a deep and well-indexed library of content for each conversational solution, as well as a thorough response-handling process – whether via Natural Language Understanding, or human support of automatically-launched programs.
Tailoring Outreach Once a Plan Has the Data to Work With
It is important to understand the challenges that members are facing, and then to target their outreach to address those barriers. Making sure to account for the hard-to-reach members in any population is vital to the approach as well. Outcome data that shows what works and what does not within certain demographics based on their SDOH impact gives the plan more insight into how to build trust within that plan-member relationship. For example, if a plan only reaches out about its benefits to their members right before they need to renew their plan, it is much less effective and meaningful than had a plan been initiating those conservations all along. But if a plan engages in those conversations about what benefits may be a good fit for that particular member based on past experiences and their demographic, then when the time comes to renew, the member is more likely to trust and value the reminder because the plan has shown to have their best interest at the core of their outreach. The member will feel more compelled to stay because they know they can rely on their current plan to address their immediate and long term needs. Maintaining the trust between plan and member is probably one of the most valuable ways conversational data can help impact the plan-member relationship.
COVID-19’s Pressure on Digital Experiences
Plans were forced to evaluate and evolve their digital outreach approach quickly with the onset of COVID-19. For a lot of plans, they had to adopt strategies to pivot into virtual care as quickly as possible. They also had to provide additional resources to help their members navigate through virtual platforms that they themselves may have been adjusting to. When a plan is able to curate a digital journey, they have an opportunity to build awareness around solutions that are relevant to members specific needs. Curating the journey helps hold their hand, helps them navigate a new digital landscape in addition to sustaining the relationship. During the pandemic, mPulse positioned the need for digital therapy to our client’s members suffering from social isolation. Before initiating an ask to the member to engage in the program, we communicated the value. This strategy was effective because we were able to educate around the need for digital therapy and gauge the members interest, which gave the member the opportunity to come to the plan on their own instead of pushing them to sign up for a new virtual care program.
As we look ahead to 2021, what we have learned in the past year and throughout our most successful programs, is that trust between member, provider, and plan is crucial, especially as we transition through one of the most pivotal moments in healthcare. But the better prepared a plan is to respond to members and their immediate needs that also doesn’t burn a lot of resources on the plan’s end, the better relationship between member and plan will be. Focusing on approach, collecting all data from those use cases, and keeping the member at the center of all strategic communication is key.