The stark reality of flu vaccines is that they save millions from illness and death, yet there remains a significant inequality in vaccine distribution, particularly affecting certain demographics. During the 2022-23 flu season, while 173.37 million Americans were vaccinated, saving nearly $2.4 billion in healthcare costs, a concerning 46% of eligible Americans remained unvaccinated.
Solving vaccine inequity requires a deeper understanding of the social determinants of health (SDoH), such as age, race, and income, which play a pivotal role in these disparities. Notably, vaccination rates are considerably lower among Black, Hispanic, and American Indian/Alaskan Native adults, with hospitalization rates significantly higher among Black adults. Furthermore, adults with lower incomes and those in the 18-49 age group are less likely to receive the flu vaccine.
Identifying and addressing the root causes of these inequities is crucial for improving vaccination rates and ensuring equitable health outcomes for all in the upcoming 2023-24 flu season.
Understanding why these inequities exist is essential when designing programs to help overcome them.
Overcoming inequality in vaccine distribution through inclusive flu outreach
Addressing vaccine inequity requires tailored strategies that specifically target the underlying causes of these disparities. The CDC highlights a lack of accessibility, misinformation, and widespread distrust in the medical system as primary reasons for flu vaccine inequities. Crafting programs that focus on overcoming these barriers is crucial to enhancing flu vaccination rates and bridging the gap in inequality in vaccine distribution.
By implementing such targeted approaches, we can work towards ensuring equitable healthcare access for all member populations.
How to address and solve vaccine inequity through enhanced accessibility
Overcoming vaccine inequity necessitates addressing accessibility challenges that disproportionately affect disadvantaged groups. Many individuals face barriers such as unreliable transportation, disabilities, limited internet access, inflexible work schedules, and language or translation issues, making vaccination access difficult. These systemic issues often fail to accommodate all members’ diverse needs and preferences, creating an unequal landscape in vaccine distribution.
Fortunately, health plans have a significant opportunity to address these challenges. By implementing programs focusing on accessibility, they can identify individual barriers and provide customized resources to facilitate access. This requires an in-depth understanding of the target audience’s specific needs.
At mPulse, we utilize internal and external data to gain comprehensive insights into member needs, allowing health plans to create highly relevant digital touchpoints. Health plans can effectively identify and address individual barriers by engaging with members through their preferred communication channels, such as SMS, email, or IVR. The right message, delivered through the right channel, in the appropriate language, and accompanied by suitable resources, is key to meeting members where they are and improving flu vaccination rates.
Learn more about how to solve vaccine inequity and enhance vaccination rates by watching our on-demand webinar, “Double Flu Vaccination Rates for Your Health Population.”
Combating vaccine inequity with effective communication strategies
In the digital age, where misinformation and knowledge gaps about vaccines are prevalent, especially post-pandemic, it’s crucial to tackle vaccine inequity by providing trustworthy and pertinent vaccine information. Misconceptions about vaccinations, particularly the flu vaccine, have increased, underscoring the need for reliable information sources.
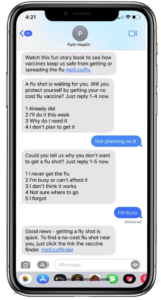
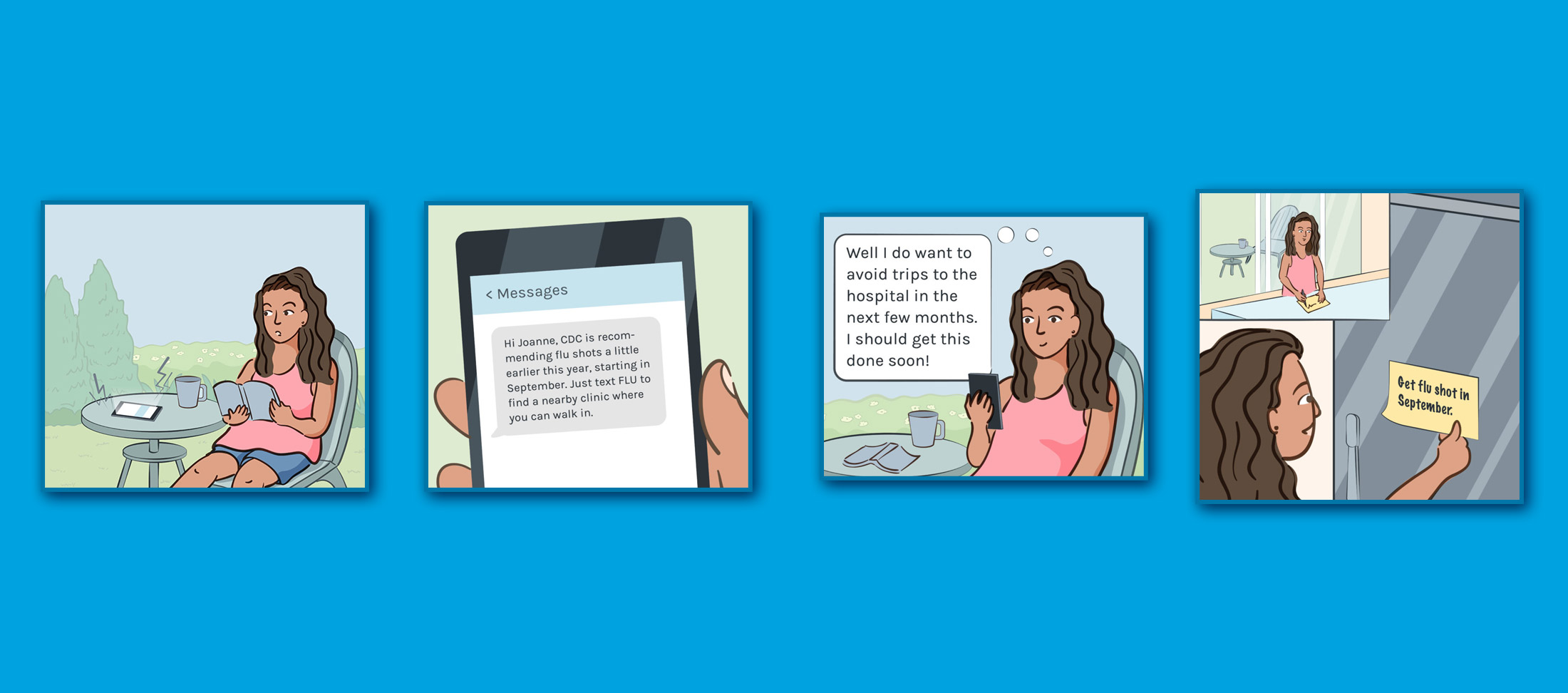
At mPulse, we aim to solve vaccine inequity by adapting the engaging formats of popular social media platforms. Our approach involves creating short-form content that is informative, educational, entertaining, and easy to consume. We focus on making content frictionless and engaging while ensuring it’s accessible to a broader audience. This includes featuring relatable characters representing diverse populations and offering multilingual options, which are vital to resonating with broader member groups and building credibility.
By sharing health content through each member’s preferred communication channels, we ensure they efficiently receive vital vaccine information. This method is particularly effective in addressing misinformation and bridging knowledge gaps, thereby playing a significant role in how to solve vaccine inequity. To see an example of how we bring this to life, view another fotonovela included in the mPulse Mobile Flu Vaccination Solution.
Building Trust to Address Vaccine Inequity
Addressing distrust in the medical system, often rooted in a history of structural racism and discrimination, is crucial in solving vaccine inequity. While health plans represent only one component of this complex issue, establishing trust with their members is vital. Utilizing digital trends for inspiration can significantly aid health plans in scaling their efforts effectively.
Creating multiple positive and meaningful touchpoints over time is key to developing and maintaining strong member relationships. At mPulse, we collaborate with health plans to provide empathetic messaging that conveys relevant and accessible information in each member’s preferred language and through the most appropriate channel. This approach helps ensure members feel supported and can rely on their health plan for essential care and resources, fostering greater trust and empowerment.
Simply notifying members about their due flu vaccines can be perceived as intrusive. Instead, our approach incorporates sensitive, culturally relevant messaging that leverages behavioral science techniques, cinematic educational content, and tailored resources. This strategy demonstrates an understanding of the member’s unique needs and genuine concern for their health.
When members feel that their health plan values and understands them, they are more likely to trust the plan and engage in healthier behaviors, thereby contributing to solving vaccine inequity.
Leveraging technology to overcome health disparities and boost flu vaccination rates
Technology is imperative in helping overcome health disparities and barriers to flu vaccinations. By leveraging innovative digital trends designed to serve vulnerable populations, health plans can begin broadening accessibility, educating and empowering members, and building trust at scale to improve vaccination rates and inspire healthier outcomes for the people they serve.
mPulse Mobile designs solutions that identify and overcome barriers to action. Our behavior change model incorporates health equity, behavioral science, and instructional strategy to deliver best-in-class outcomes.
Contact us to learn more about how our flu vaccination solution can help overcome vaccine hesitancy for your members.