In an era where communication is king and technology reigns supreme, SMS (Short Message Service) has emerged as a pivotal tool in healthcare outreach. With nearly 6 billion text messages exchanged daily in the United States alone, the potential of SMS in healthcare consumer engagement is unparalleled.
However, harnessing the full power of healthcare SMS for outreach requires more than just sending generic messages. It demands a nuanced understanding of best practices to truly connect with members and drive positive health outcomes. From personalized messaging to maximizing call-to-action completion rates, mastering SMS best practices is essential for any health plan striving to optimize member engagement and deliver impactful healthcare outcomes.
Join us as we explore the intricacies of SMS best practices in healthcare outreach and delve into five key healthcare SMS strategies proven to
- enhance SMS engagement,
- optimize member interactions, and ultimately
- drive better healthcare outcomes.
Understanding the growing potential of SMS
From its humble origins in 1992, SMS has evolved into a cornerstone of connectivity, facilitating billions of daily interactions across the country. In fact, SMS is today the most common and widely used form of communication in the United States, and it has been since 2007 when the number of text messages surpassed those of phone calls.
Within healthcare, SMS has reshaped how healthcare organizations engage with patients. With the advent of multimedia messaging services (MMS) and rich communication services (RCS) functionality, the capabilities of SMS have expanded exponentially, offering personalized and interactive touchpoints for patients.
One significant advancement in recent years has been the integration of artificial intelligence (AI), which marked a new era in healthcare communication. Healthcare organizations can now deliver tailored support and guidance to patients by leveraging AI-driven conversational interfaces. This has revolutionized the member and patient engagement landscape and realized remarkable outcomes for engaging hard-to-reach and diverse populations.
Navigating Engagement and Outcomes
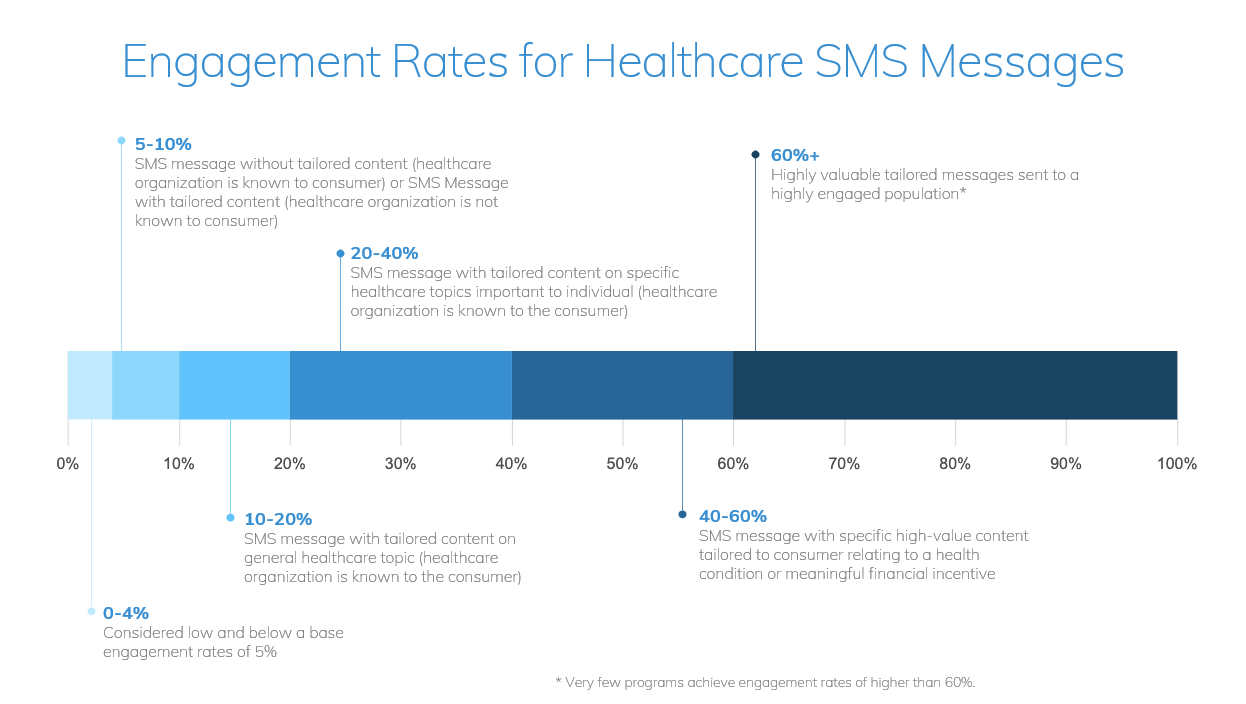
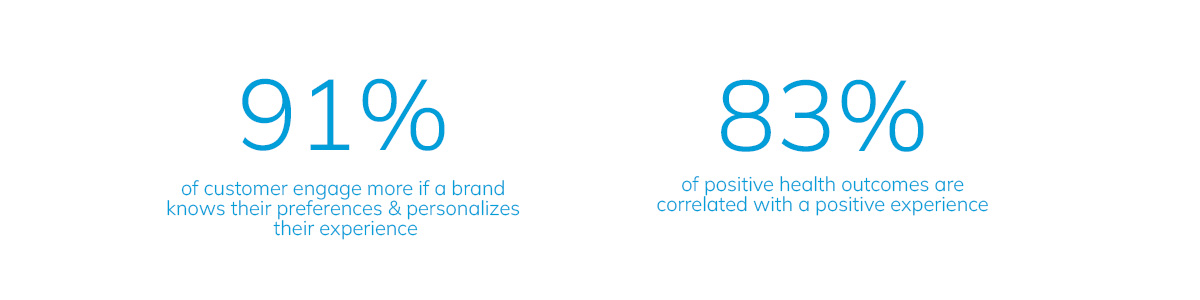
Despite so many technological advancements, the essence of effective SMS communication for healthcare remains the same – its ability to engage members and patients meaningfully. Generic messages often fail to capture recipients’ attention, resulting in low engagement rates, and it’s clear that personalization is key to driving meaningful interactions.
On average, text messages have a 99% delivery rate, with 95% being opened within 5 minutes. However, receiving a text from your health plan isn’t quite as exciting as receiving a text from your best friend or significant other. This is why it’s imperative health organizations schedule health SMSs that are personalization and meaningful dialogue to maximize engagement.
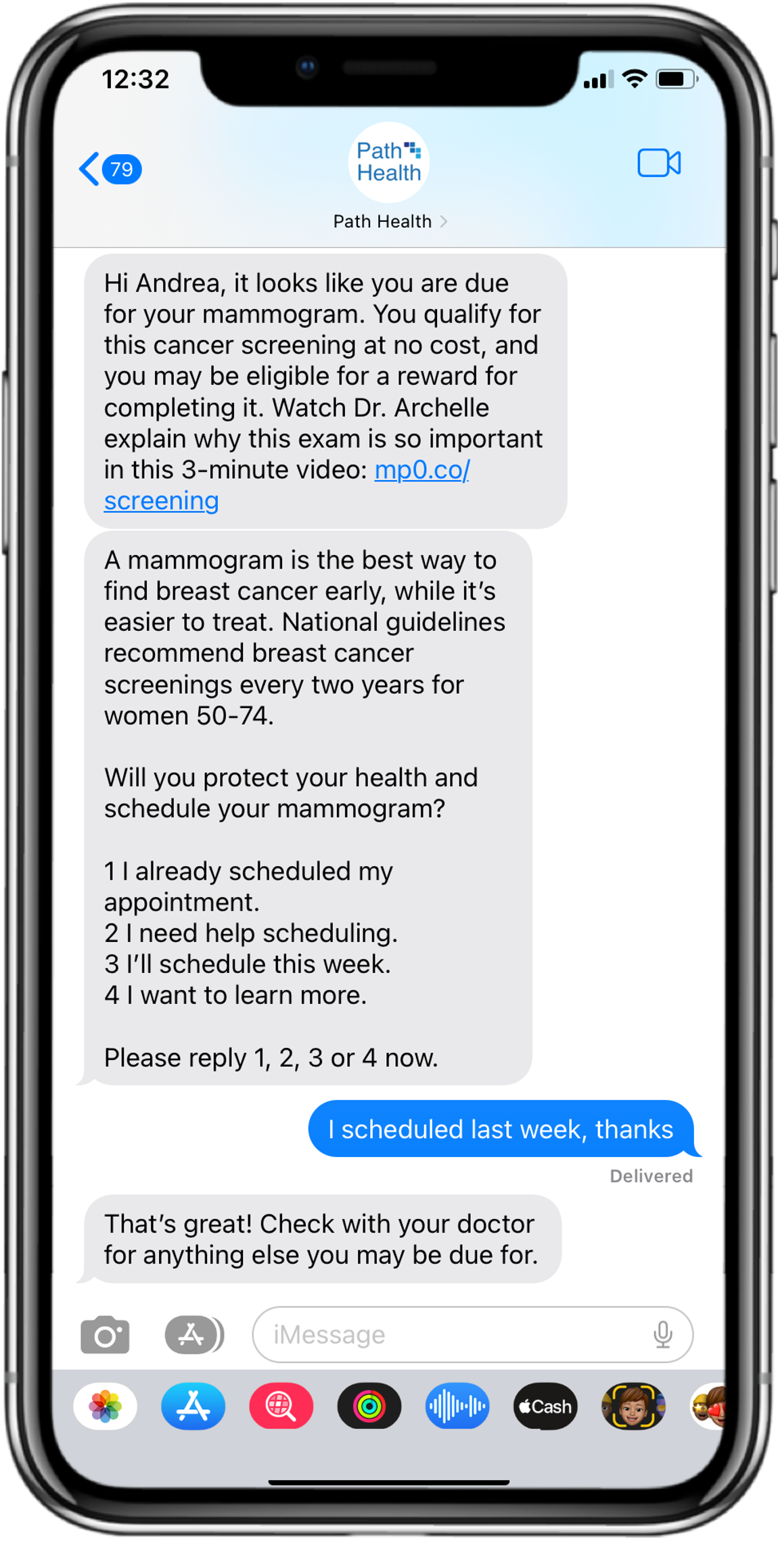
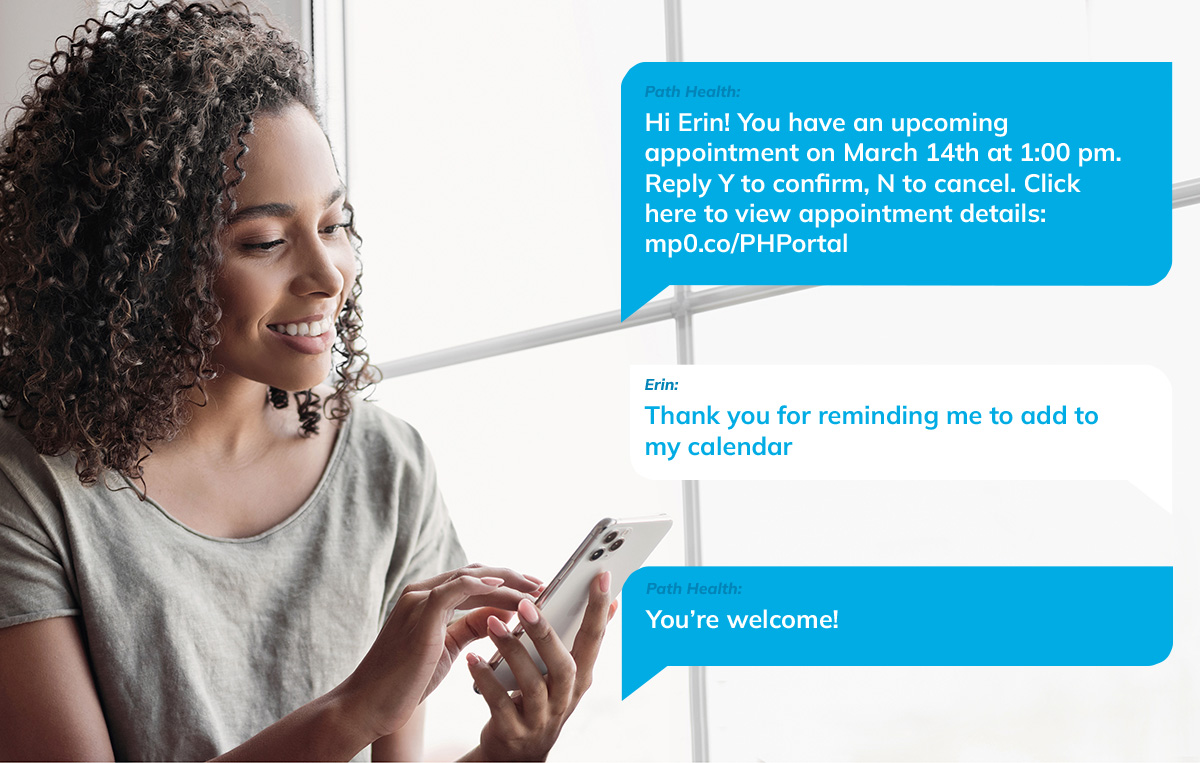
Imagine receiving a text message from your healthcare provider addressed to you by name, offering tailored guidance based on your specific needs and preferences. Going even further, picture being able to respond and converse through text messages with your health plan or provider and being sent helpful videos and lessons in response to your concerns. This personalized approach enhances engagement and fosters a sense of trust and connection between patients and the healthcare organizations serving them.
Furthermore, the impact of personalized healthcare SMS content extends beyond mere engagement metrics. Healthcare organizations have witnessed tangible improvements in health outcomes by delivering targeted messaging. From a 10pp improvement in colorectal cancer screenings to enhanced access to care measures, the power of tailored SMS content is undeniable.
Embarking on a journey of best practices
As healthcare organizations navigate the realm of SMS communication, embracing best practices becomes essential. It’s not just about SMS templates for health insurance or other medical solutions but crafting meaningful interactions that resonate with patients.
Five key practices to optimize healthcare SMS outreach efforts
- Establish trust for effective communication
Trust is the cornerstone of effective SMS communication for healthcare. By introducing yourself and explaining the purpose of the message, you lay the foundation for a meaningful dialogue with patients.
To do so, begin by addressing recipients by name and introducing yourself, then explain the purpose of the message clearly. Not only does this approach confirm the message is intended for the recipient, but by letting the consumer know you care about them and their health, you begin to lay the foundations for a meaningful relationship that will improve the likelihood of health action and, thus, member retention.
Another important consideration, although somewhat more technical in nature, is your “sender number”. Be consistent with this. Using a standard shortcode will establish trust with the service provider, preventing your messages from being blocked as spam. You can also send your members a virtual contact file (VCF) card, a great way to get all your information into your members’ phones and ensure your messages are automatically directed into their “known inbox”.
- Empower members to take action
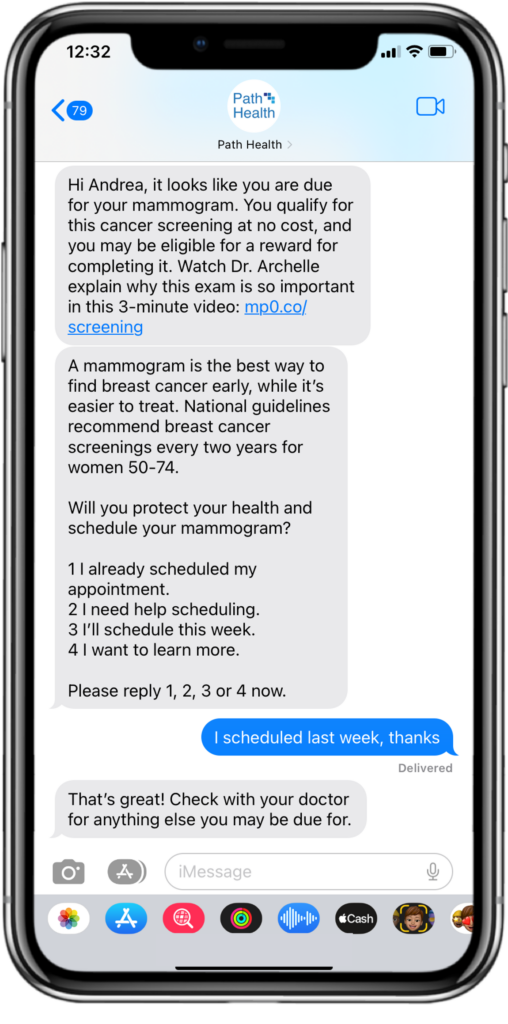
Healthcare messages should be structured to enable members to take immediate action. Provide clear instructions and mechanisms for them to follow through on desired actions, such as scheduling appointments or accessing resources.
SMS allows you to use clickable links, making it easy to direct members to relevant materials or services. These branded links enhance trust, as members can see where they’ll be going before they tap on a link, but they also mean you’ll be able to track interactions at the member level for valuable, near-real-time insights.
Beyond that, you must enable your members to continue interactions. This will allow you to address any barriers preventing them from taking action and empower patients to navigate their healthcare journey seamlessly.
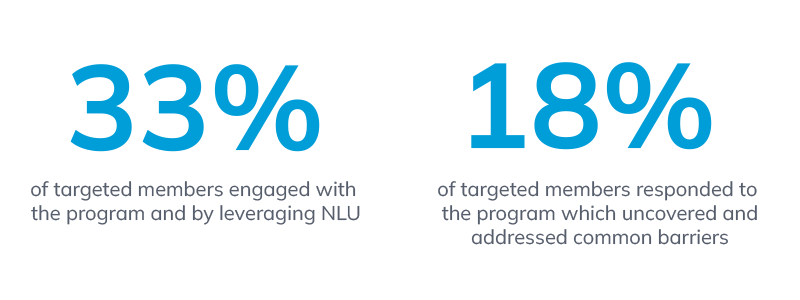
Conversational AI and Natural Language Understanding (NLU) enable members to reply with questions and for the technology to read a message and provide a relevant response that addresses their concern and motivates them to engage in the health action you’re driving by providing the tools they need.
By responding in a natural conversational way, you can continue the conversation, uncover barriers, and get the member or patient one step further toward taking the desired action. In turn, your members will feel seen, heard and valued, resulting in a far more pleasant consumer experience overall.
- Give your content a boost
Personalizing your content not only builds trust but also allows you to tailor messages to the specific needs and preferences of each recipient. By tailoring content to address demographic information and social determinants of health, you can enhance engagement and drive positive health outcomes.
Incorporating multimedia elements into SMS, such as streaming health content, further boosts member engagement. Visual and narrative communication, particularly through video, captivates recipients, fostering a deeper connection and understanding of healthcare information.
A recent A/B test including embedded streaming health content in SMS resulted in a 270% increase in click-through rates and engagement. At the same time, the neuroscience around narratives shows that people retain about 7-12 times more information when it’s told as a story.
- Speak the same language as your members
Health plans often cater to diverse populations with varying language preferences, which can present a challenge. However, there’s no denying that effective communication involves speaking to your members in their preferred language.

Communicating with members in their native language is one of the most high-value things you can do for positive engagement. Fortunately, with NLU, it’s possible to identify and respond to your members’ language choices.
Adjusting to a patient’s language encourages positive engagement and valuable relationship creation
For example, if someone responds to you in Spanish, respond to them in Spanish to let them know they can change their language from English simply by replying with the word “español”. Once you’ve confirmed their language, you can update their language preferences automatically to ensure that all future communications with them will also be in Spanish.
- Check the compliance box
Managing opt-ins and opt-outs is not just a best practice; it’s a legal requirement under the Telephone Consumer Protection Act (TCPA).
Ensure compliance with regulations by promptly honoring requests to opt-out. We all know what it’s like when you’re inundated with messages – sometimes people may reply “stop” simply because they’ve received one text message too many that day or because they don’t understand who the sender is. To overcome that particular challenge, make sure you always provide a way for members to opt back into the communication channel if they change their minds.
Understandably, healthcare organizations may have concerns about TCPA compliance, but if you’re looking to use messaging for the first time, rest assured that text messaging programs offer some definite advantages over other forms of communication.
Elevate your SMS strategy for better healthcare outcomes
In the evolving landscape of healthcare communication, healthcare SMS stands out as a versatile and effective tool for health plan outreach. Adopting SMS best practices is essential for any health plan aiming to unlock the full potential of this powerful communication tool, transform member engagement and drive positive health outcomes.
Our recent webinar on “Leveraging SMS for Health Plan Outreach provides even more in-depth insights and practical strategies.
To delve deeper into the world of SMS best practices and get to the bottom of some common myths about the TCPA, download the full webinar, where industry experts discuss real-world outcomes and practical tips for success.
To learn more about mPulse’s digital health solutions and outcomes, contact us at info@mpulsemobile.com.