Now that the dust has settled and we have all had a chance to unpack the 1,300+ pages of the 2025 Final Rule, the real work begins.
Many aspects of this final rule were anticipated and some long overdue, this Final Rule represents a powerful shift in the continued pursuit to expand access, strengthen beneficiary protections, address (not just identify) social needs, improve the quality of care and member experience, and…gulp…shift dollars back into the Medicare Trust Funds.
Stars, HEDIS, Risk Adjustment, and senior market supporting teams are all here because they are not afraid of a little work, and they are passionate about improving the lives of the beneficiaries they serve. So, we do what we do every year, roll our sleeves up and get to work.
That’s exactly what the mPulse teams have been doing since the release of the Final Notice. We started our strategic conversations around much of this work during the Proposed Rule and Advance Notice and have already implemented a number of changes and updates to our solutions and products so we can better support our health plan clients tackle the big stuff.
Whether they were new, codified, or just now at our ‘front door’ topics, we’ve summarized a handful of key items that we’re getting to work on and providing some best practices, tips, and strategies for plans to address them head on.
1. Medication Therapy Management (MTM)
Expanding MTM program eligibility criteria by:
- Adding HIV/AIDS to the core condition list
- Including all Part D maintenance drugs
- Revising the cost threshold calculations
mPulse’s Strategic Approach
Chapter 7 of the Prescription Drug Benefit Manual (as noted in 30.3 & 30.7) states CMS expects sponsors to have procedures in place to drive participation and follow-up with beneficiaries that do not respond to initial offers and to consider using more than one approach, when possible, to reach all eligible patients.
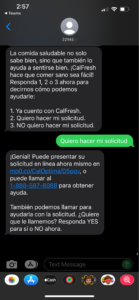
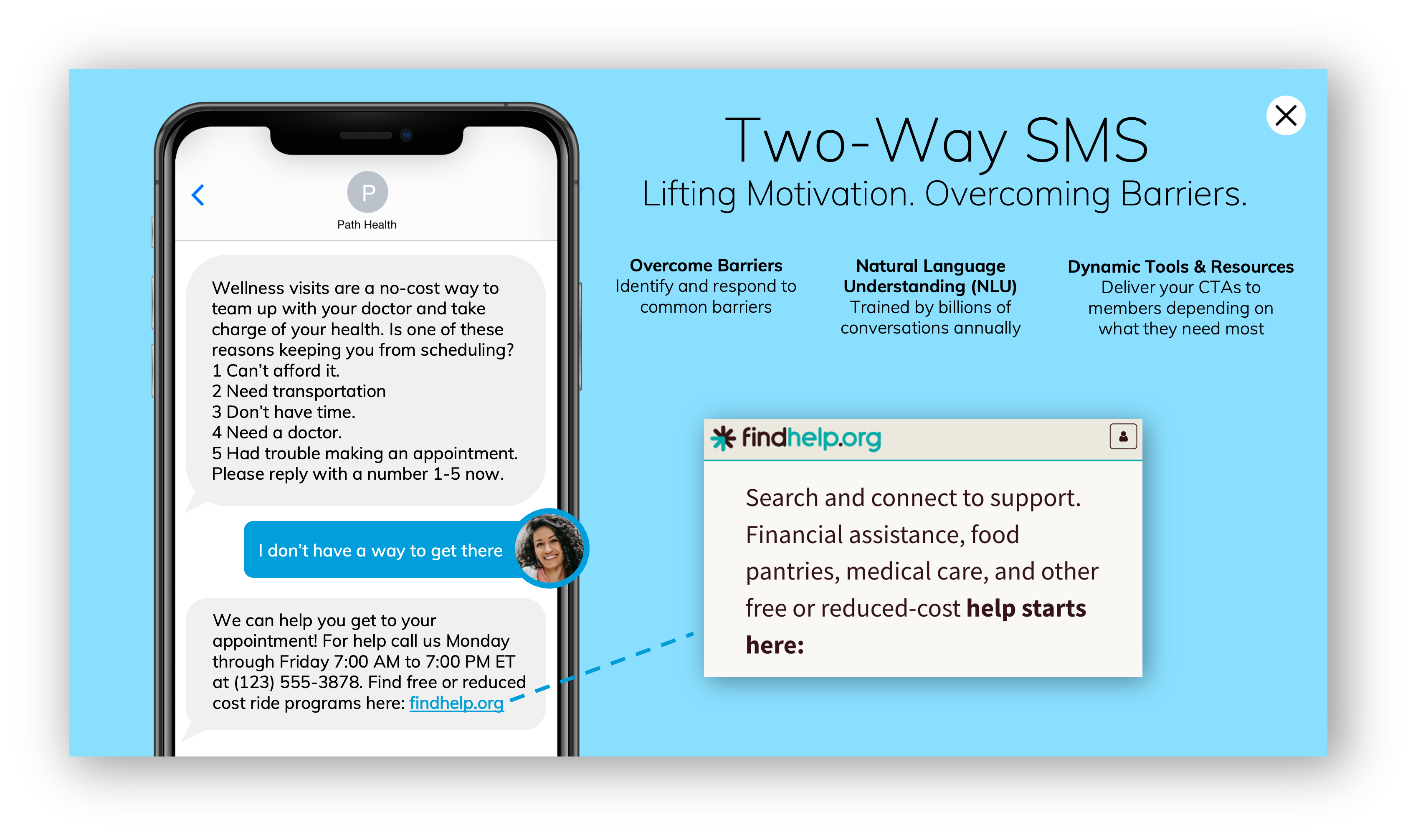
Offer an omni-channel approach to reach all eligible members, anticipate your members needs by reminding them the service is a covered benefit and helping them prepare for the CMR, and reinforcing the benefit of routine medication reviews.
Remember, adding new channels or additional supports to help members complete their CMR can be added to your MTM program throughout the year.
2. Health Equity Index (HEI) and Reward
Data collection beginning with calendar years 2024 and 2025 will shape the 2027 Star Ratings and impact the 2028 payment year. Ratings and reward will be determined by not only performance but enrollment thresholds within dual eligible, low-income, and disabled beneficiary populations.
mPulse’s Strategic Approach
With expanded LIS eligibility extended to individuals with incomes up to 150% federal poverty level (FPL) in 2024, some beneficiaries may not even know they qualify. Plans will want to make sure all of their eligible members have applied and qualified for subsidies. Not only should all beneficiaries have the protections available to them, plans can’t afford to miss those HEI enrollment thresholds whenever and wherever possible.
There are a few steps to a successful approach:
- Use predictive models and analytics to identify members who may be eligible for but not currently receiving extra help.
- Develop an omnichannel engagement strategy to inform members of the income thresholds, provide them with information and support on how to apply.
- Be prepared to support members who may not qualify by offering additional plan, local, state, or federal resources. And help any new LIS members understand and utilize their new benefits fully.
Want to learn more about addressing health inequities? Download the white paper »
3. Mid-Year Enrollee Notification of Available Benefits
In addition to the new requirement to submit utilization and costs data in EDS, CMS will require plans to provide beneficiaries with a mid-year notification of all unused supplemental benefits. Each notification must be personalized, include details about the unused benefit including applicable cost-sharing details, information on how to access, required network information, and a contract center number for additional assistance.
mPulse’s Strategic Approach
Getting the right benefits, supplemental and otherwise into the right hands of the right members isn’t always easy. We often cast a wide net and hope standard means of communication (EOCs, SOBs, landing pages etc.) are sufficient. Actions taken by CMS in this area prove that it is not enough, and many benefits are being underutilized or not used at all.
Start looking at your membership now, even without robust supplemental benefit utilization data, use claims and encounter data to create need-based populations who could most benefit from your supplemental offerings. Putting in efforts now will pay off in AEP and OEP when your members can be prompted to benefits that resonate with them both socially and clinically. And if done well, could not only cut down on the number of benefits you’ll need to notify them about come mid-year but support your broader retention and satisfaction efforts.
4. Member Experience and Access Measures, CAHPS & HOS
- Member Experience and Access Measure Weights Reducing from 4x to 2x for Stars Year 2026
- Improving or Maintaining Mental Health & Improving or Maintaining Physical Health Weight Increasing from 1x to 3x each for Measurement Year 2025
mPulse’s Strategic Approach
CMS realigning the weight of experience and access (aka administrative) measures while still providing beneficiaries with a ‘voice’ that will hold plans accountable and impact ratings, these measures will still account for nearly 20-30% of the overall Star Rating over the next few years (trending to less moving forward).
After being moved to the display page due to data disruption during collection years during the pandemic, the two longitudinal HOS measures will be returning to their original weights.
Weight shifts and temporary retirement to the display page should never be an excuse to ease up on overall strategy for any measure category. There is no one-size-fits-all approach to CAHPS and HOS, rather a data driven and personalized approach to understand what is working, what is not, who is in need, who is not, who is aggrieved and at risk to respond negatively and so on. Leverage data collected through regulatory and off cycle surveys along with health plan data, both clinical and non-clinical to develop an informed strategy for outreach. Deliver live agent calls to those most at ‘risk’ and deploy high-touch digital communications to your other segments. This allows you to cover the largest volume of membership without sacrificing personalization and service recovery.
5. Inflation Reduction Act – Part D Redesign
- Medicare Prescription Payment Plan (M3P)
- Elimination of Coverage Gap
- Part D annual out-of-pocket maximum reduced to $2000
mPulse’s Strategic Approach
CMS continues to strengthen protections for individuals who rely on Part D coverage. Between the 2022 IRA and 2025 Final Rate & Rules and beginning on January 1, 2025, beneficiaries will have a lower out of pocket maximum, no coverage gap phase, and the opportunity to spread the cost of their drugs out over the year with monthly average payments instead of all at once at the POS.
While all favorable financially to beneficiaries, some of these changes are bound to cause confusion. Even when a 2025 copay or coinsurance is less than it was in 2024, beneficiaries will still call and ask why. The M3P is likely to cause confusion for not only your members, but your call centers, and network pharmacies. Relying on traditional means of communication won’t be sufficient. Highly tailored and personalized communications to members who may need it the most (high spend and utilizers, early donut hole goers in 2024 etc.) will not only help them navigate this new Part D world, but it should also reduce the need for inbound calls, and ideally yield favorable satisfaction and retention for CAHPS and OEP.
6. Colorectal Cancer & Breast Cancer Screening
- Expand Screening Age for Colorectal Cancer Screenings
- Gender Neutral Terms for Breast Cancer Screening
mPulse’s Strategic Approach
In alignment with NCQA, CMS will also expand eligible member populations to cover those aged 45-49 for the colorectal cancer screening measure and begin using gender neutral terminology for the breast cancer screening measure.
While changes to Stars often lag other measures stewards (NCQA, PQA, USPSTF) it shouldn’t necessarily stop plans from early adoption of some changes. The two listed above are a prime example. As soon as available and aligned with preventive coverage, new age bands should be included in educational outreach. And we don’t necessarily need a measure steward to tell us when to use gender neutral terminology.
Best practice here is to incorporate these changes early on, educate your member facing teams, update your stock and custom printed materials, as well as digital communications and landing pages.
If you’d like to learn more about how we are applying DecisionPoint by mPulse predictive analytics and mPulse digital engagement strategies to these and other changes across all lines of business, reach out to me directly or visit our solutions page at www.mpulse.com.
MTM – Rx Drug Manual: https://www.cms.gov/medicare/prescription-drug-coverage/prescriptiondrugcovcontra/downloads/dwnlds/chapter7pdf
Supplemental Bene Reporting Requirements: https://www.cms.gov/files/document/cy2024-part-c-reporting-requirements.pdf