Breast cancer remains a leading cause of cancer death amongst women in the United States. And while cancer rates have slowly declined, there are still barriers amongst diverse communities that prevent many of them from seeking timely and potentially life saving screenings.
Black women have a 40% higher mortality rate for breast cancer, while their five year survival rate is 81%; nearly 11% lower than white women. Women with a disability are also less likely to receive breast cancer screenings due to various barriers, including accommodations for their disabilities, and Hispanic women are 30% less likely to be screened compared to white women, yet breast cancer is the most common cause of death in Black and Hispanic women between the ages of 45 to 60 years old.
Proactively reaching out to members due for screenings and educating them on the importance of preventive care is critical to ensuring they receive the best outcomes and care. Unfortunately, when barriers such as poor experience, lack of access and respect, and costs are coupled with conflicting cultural beliefs, it becomes increasingly challenging to increase breast cancer screening rates amongst diverse communities.
However, through the power of behavioral science, technology, and health literacy tools, we can craft effective programs which remove at least some of these barriers to increase breast cancer screenings in at-risk populations.
Top 4 Challenges to Increasing Breast Cancer Screenings
Challenge 1: Influencing Members to Take Action
To influence people and drive positive behavior change, you first have to understand their individual preferences and what drives them. Behavioral science explains to us why people do the things they do. By taking and using these principles, we can engage with members and patients in ways that make it easier for them to take action—thereby ensuring they complete their breast cancer screenings.
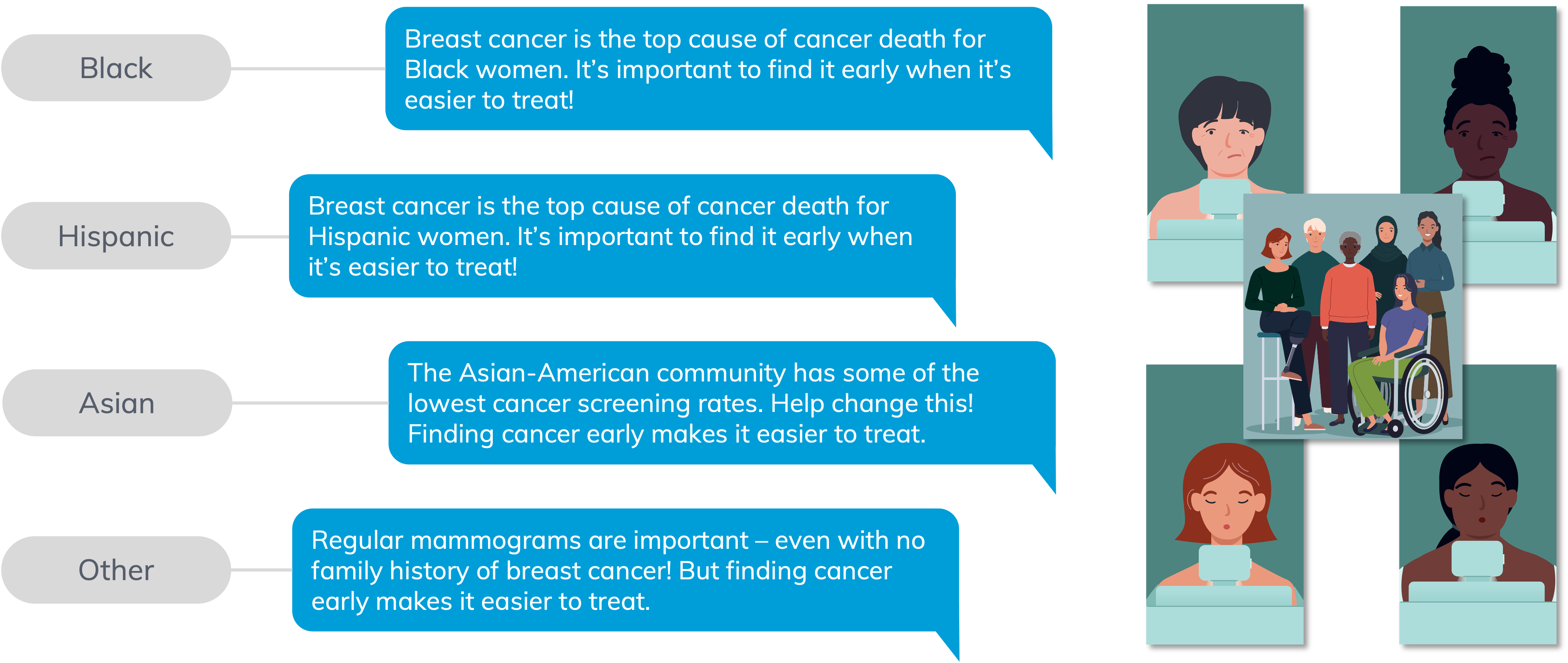
One behavior change technique mPulse utilizes in our breast cancer screening program is social proof. Most people are heavily influenced by what others think, say, or do, especially when they see people who resonate with them. Members are motivated to schedule and attend breast cancer screenings when they hear from others similar to themselves willing to discuss culturally sensitive topics. It encourages diverse groups of women to schedule screenings because they’re learning from the experience of peers like themselves.
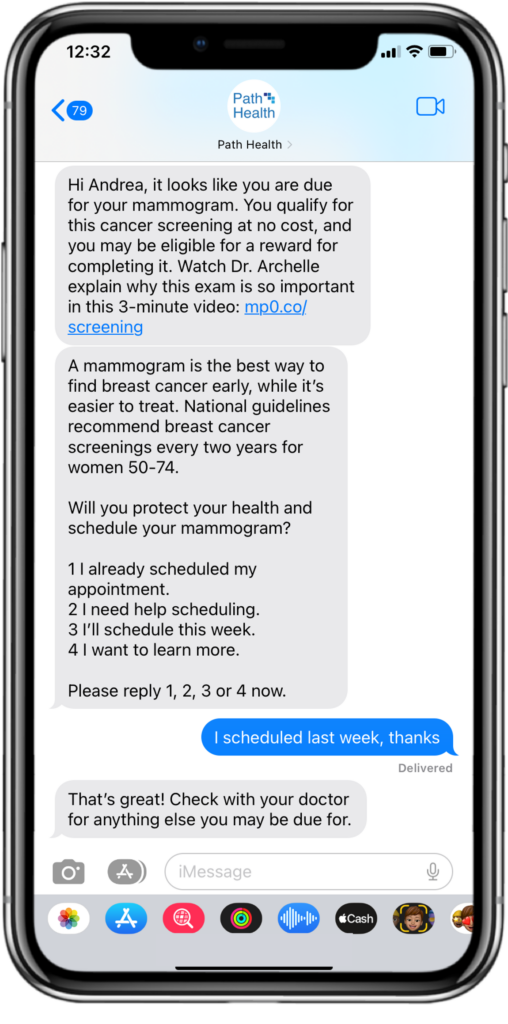
Below shows an example of activating social proof. When you show a member that other women like them do get breast cancer screenings and remind them that mammograms are normal and common among similar women, it’s more likely to have an impact.
Challenge 2: Identifying and Breaking Down Members Barriers
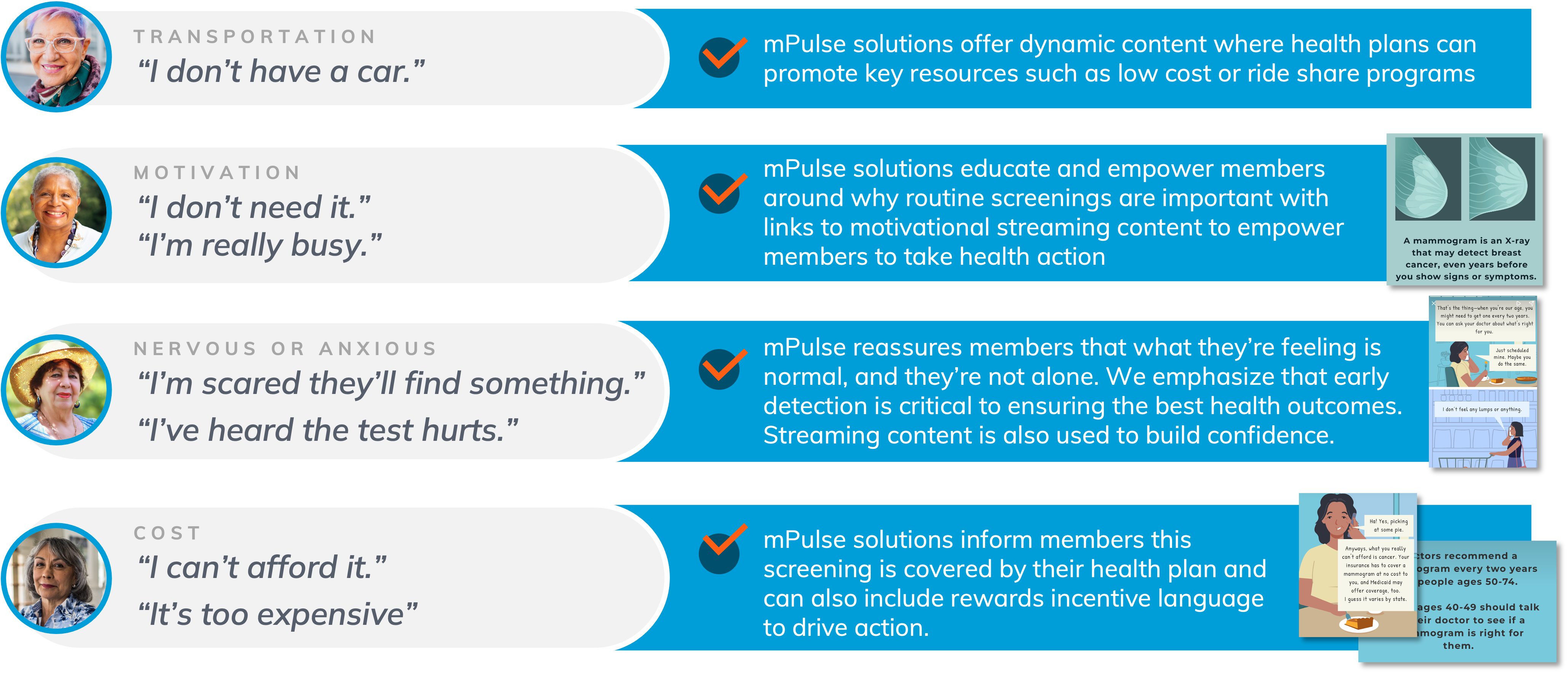
Getting the message to your members unfortunately doesn’t necessarily mean they will act on it. There are many barriers members face to accessing healthcare – transportation issues, lack of understanding around their health needs, the cost of healthcare, and more.
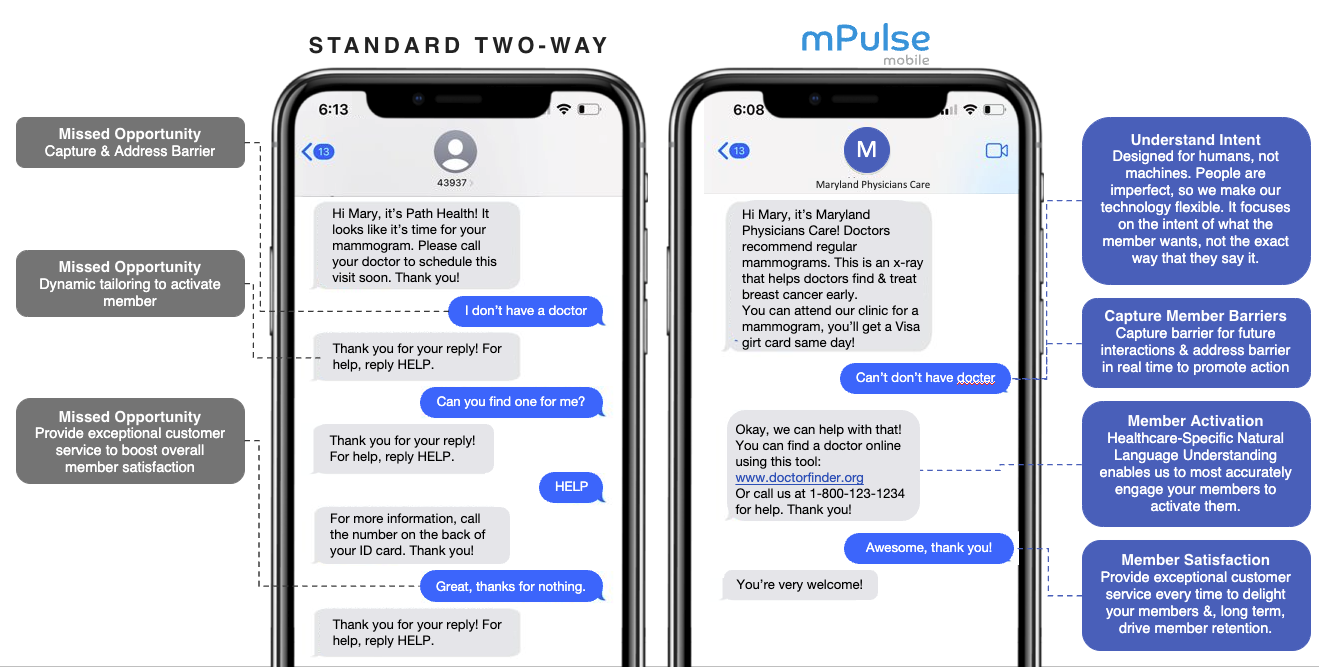
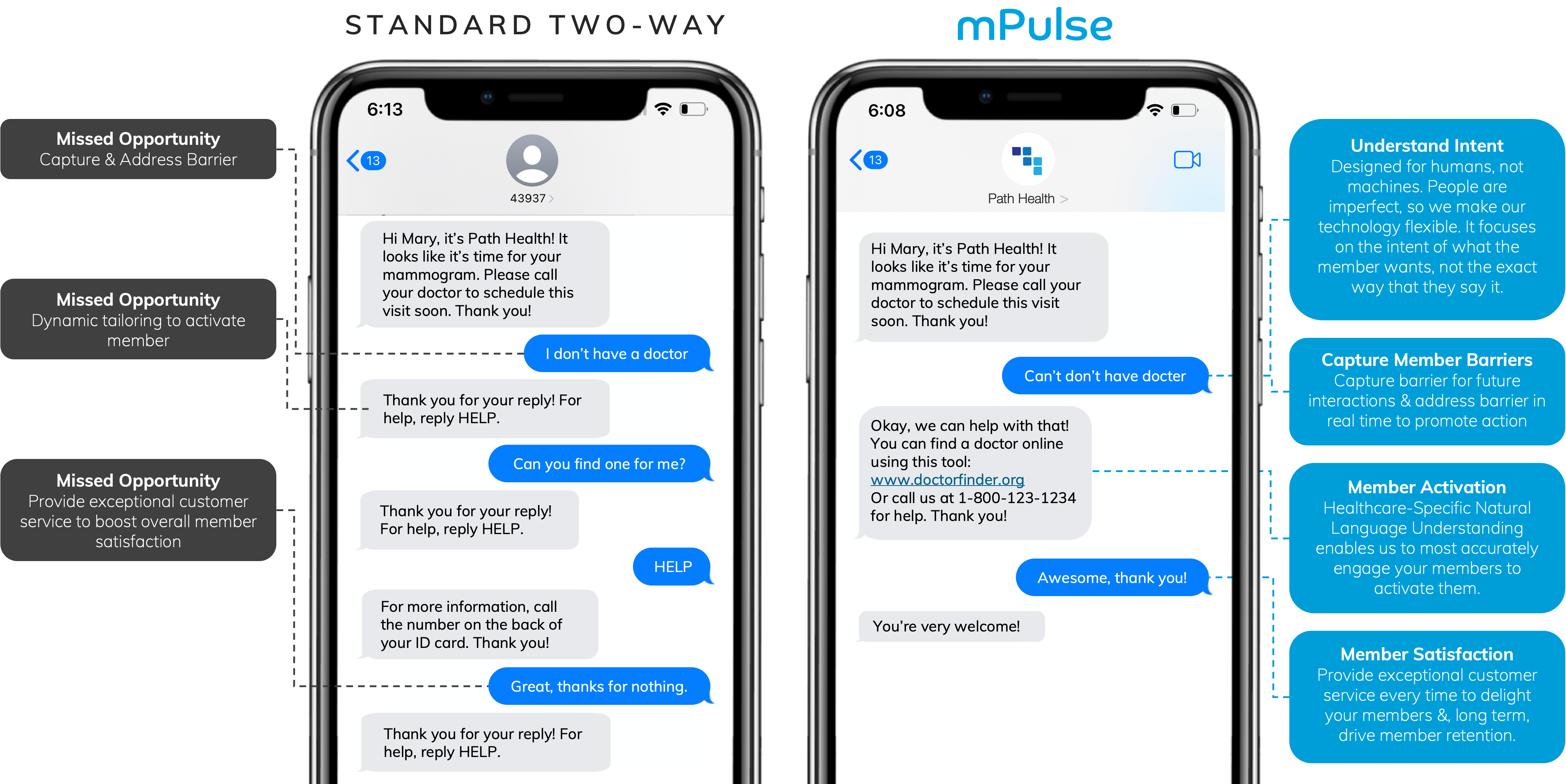
Using Natural Language Understanding (NLU) and conversational AI, you can not only understand the response of each member to identify their specific barrier, but you can also respond automatically and in real-time to address barriers at scale.
Our advanced capabilities decipher complex replies, including typos, in 7+ languages* at any point throughout the member journey to provide configurable resources and support when and where it’s needed most.
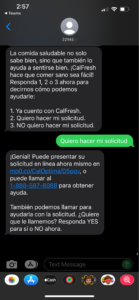
For example, if people have indicated that they’re unable to get to their breast cancer screening appointment, our technology is able to understand that and respond with rideshare resources and a phone number to request one (which reduces the perceived effort of completing this action).
By doing this, you are improving the health of your population as a whole, while continually creating personalized touchpoints that build relationships and trust with each member, enhancing retention and loyalty.
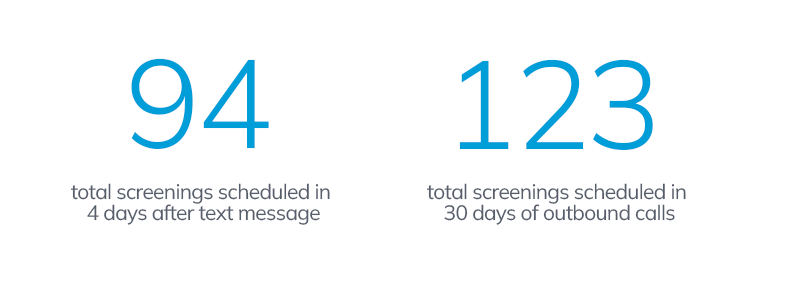
Case Study: Leading MCO Deploys Barrier Identification Program
To identify and address barriers to breast cancer screening, one leading MCO Health Plan partnered with mPulse to send tailored SMS messaging to members who hadn’t scheduled their annual mammogram. Leveraging two-way dialogue, their responses were analyzed through the use of NLU and appropriate, relevant automated replies were sent to help members overcome barriers such as fear, being “too busy”, or even not having access to transport or childcare.
For this use case, we were able to identify the largest barriers based on responses for their member population. See below for example dialogue* and most frequent barriers gathered from response data.
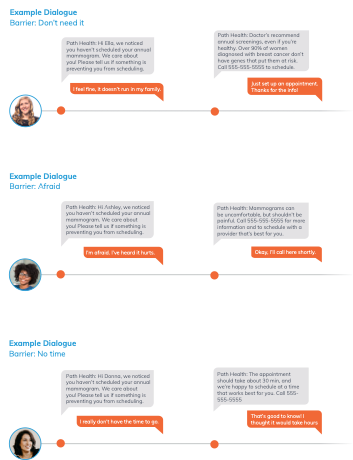
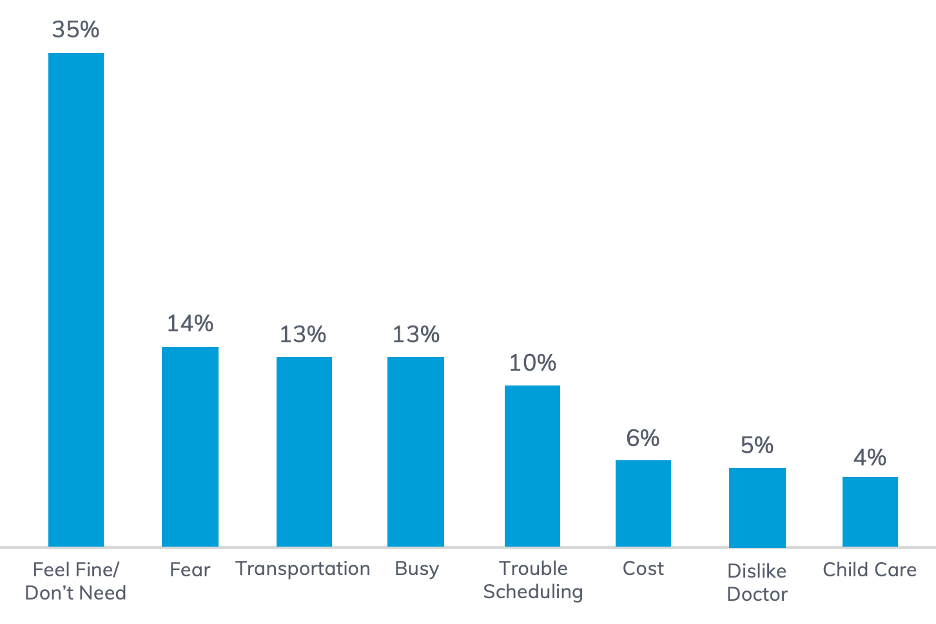
By analyzing member response data, plans can begin implementing the resources and education needed to further help members overcome barriers.
If people don’t see screenings as being important, or worth their time, we need to educate members by providing relevant information that explains why they’re important and empower them to take health action. Critically, we need to lower the perceived effort involved, let them know their plan is there to help them complete it and try to drive home the message that cancer treatment is more effective with early detection.
Supporting barrier identification with relevant responses and additional calls to action will continue to reinforce healthy behaviors throughout the member journey, while reinforcing self-efficacy.
Challenge 3: Improving Health Literacy to Close Gaps
Health literacy is the degree to which individuals have the ability to find, understand, and use information and services to inform health related decisions and actions for themselves and others. When low health literacy is not addressed, it’s a problem.
So how do we create more equitable solutions?
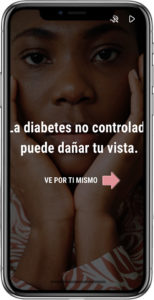
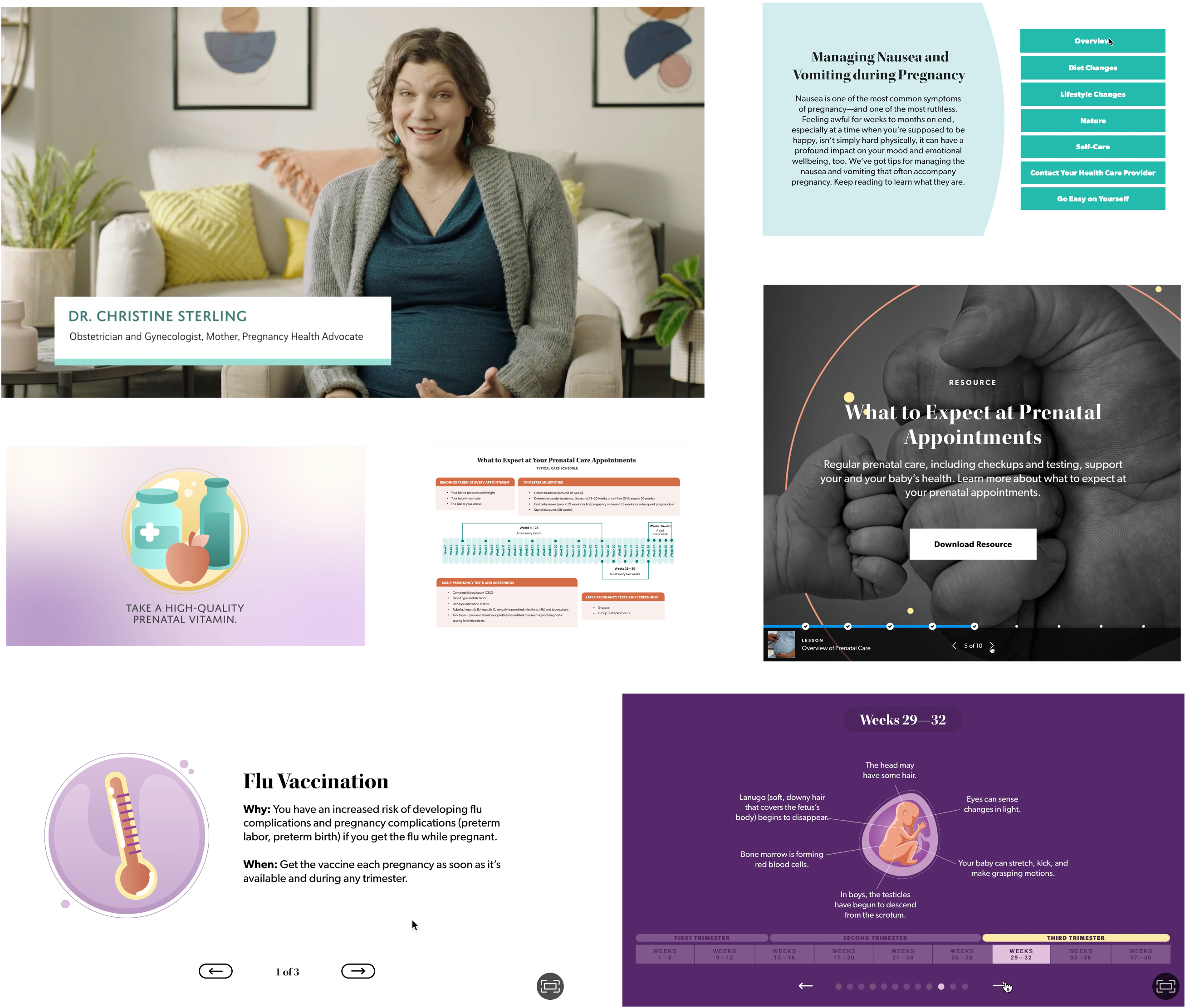
Our team of instructional writers and designers produce high-quality content designed to build health literacy at scale. Our breast cancer streaming content in particular makes use of visuals and language that makes members feel represented in the story. So different pieces of the stories will actually change to be more reflective of the population we’re speaking to, depending on the audience and the data we receive on race and ethnicity.
Our Behavioral Science team also crafts dialogues by pulling research that studies population demographics, belief systems, health attitudes, and more. Leveraging this data allows our communication to resonate with your unique population, build health literacy and inspire behavior change through personalization.

Challenge 4: Addressing Health Inequities to Overcome Barriers
Unaddressed health disparities are going to cost almost $1 trillion by 2024. Ignoring health inequities means more people are calling out sick and means more money lost, not to mention the loss in economic productivity.
By leveraging digital strategies for member engagement, however, and focusing on key factors such as social determinants of health (SDoH), cultural competency, accessibility, and health literacy, it’s possible to tackle these challenges meaningfully and respectfully.
mPulse’s breast cancer screening program takes this all into account and tailors the content to fit the needs of each individual member. Thoughtfully incorporating streaming content at key moments serves to build trust, overcomes barriers, and educates members, while portraying characters of different races depending on member data to ensure the content resonates and feels personalized to each member.
Creating Healthier Populations, One Member at a Time
While breast cancer disproportionately affects low income, racial, and ethnic minorities populations it is possible to reduce cancer-related health disparities, with a few simple enhancements to your existing strategies.
From framing choices using social proof, to ensuring your member populations are represented in your messages, and taking the time to listen to their challenges, you can overcome physical, psychological, social, or cultural barriers, provide solutions and ultimately improve your breast cancer screenings in underserved populations.
Many of these suggestions are simple content improvements that can be added to an existing system, evaluated and adjusted with little cost but by crafting personalized member journeys, we can help build relationships that uncover barriers and facilitate healthier behavior change at scale.
To learn more about mPulse Mobile’s solutions and programs, contact us.
*Example dialogues created for the purpose of this blog.
Improving Health Outcomes// Creating Healthier Populations, One Member at a Time
















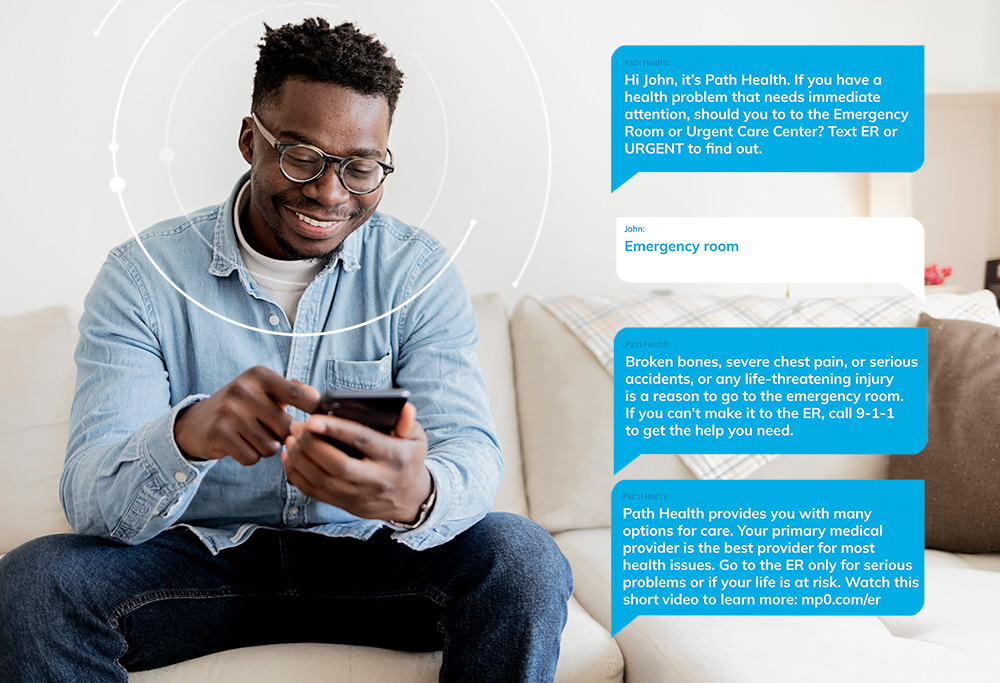



 We know 97% of American adults own a mobile phone, so leveraging this communication channel to reach more consumers is a great place to start. Scaling this resource requires automation, and to avoid abrasion, we lean on conversational AI and Natural Language Understanding (NLU) to direct consumers to the right tools and resources.
We know 97% of American adults own a mobile phone, so leveraging this communication channel to reach more consumers is a great place to start. Scaling this resource requires automation, and to avoid abrasion, we lean on conversational AI and Natural Language Understanding (NLU) to direct consumers to the right tools and resources.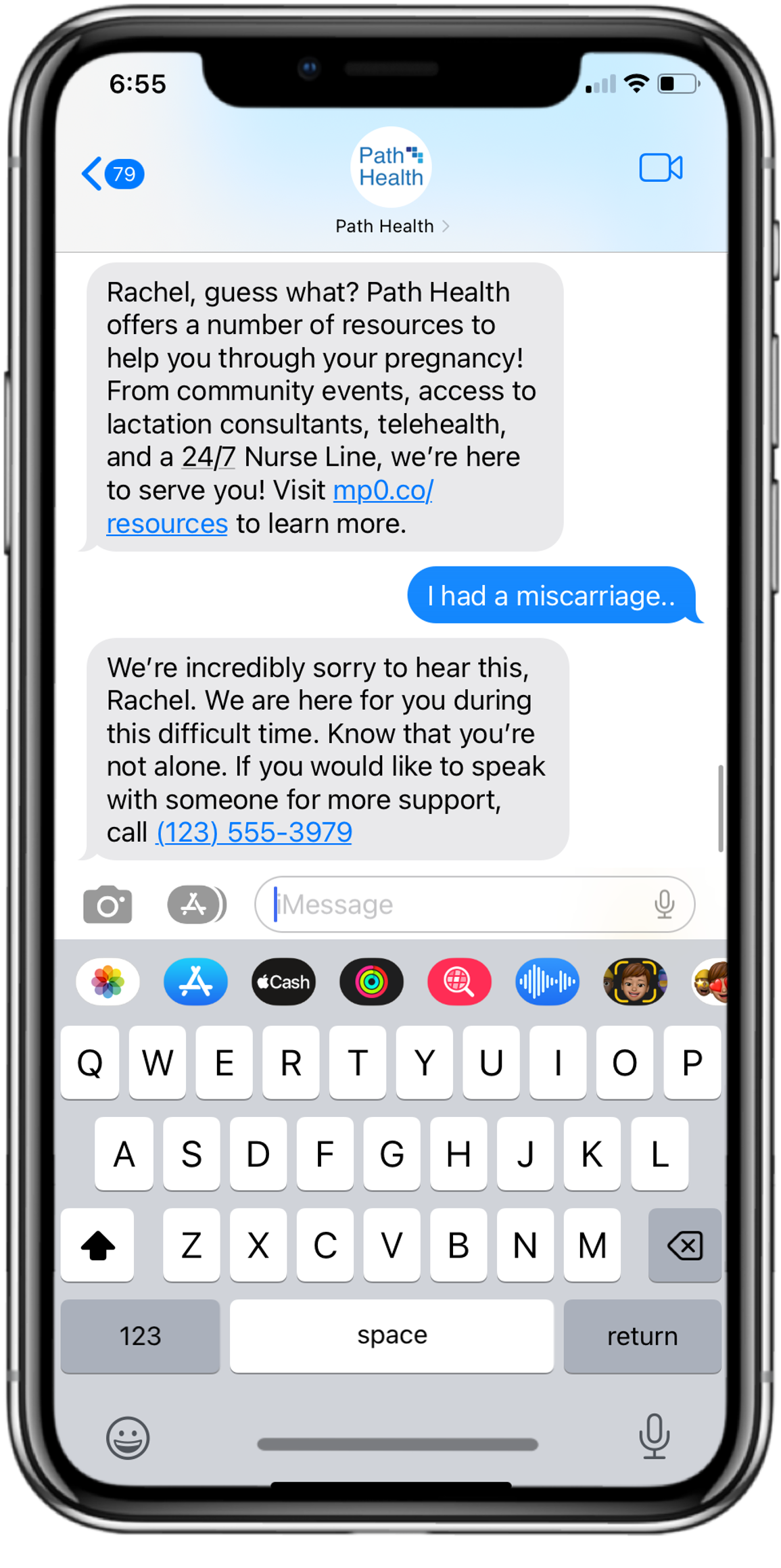


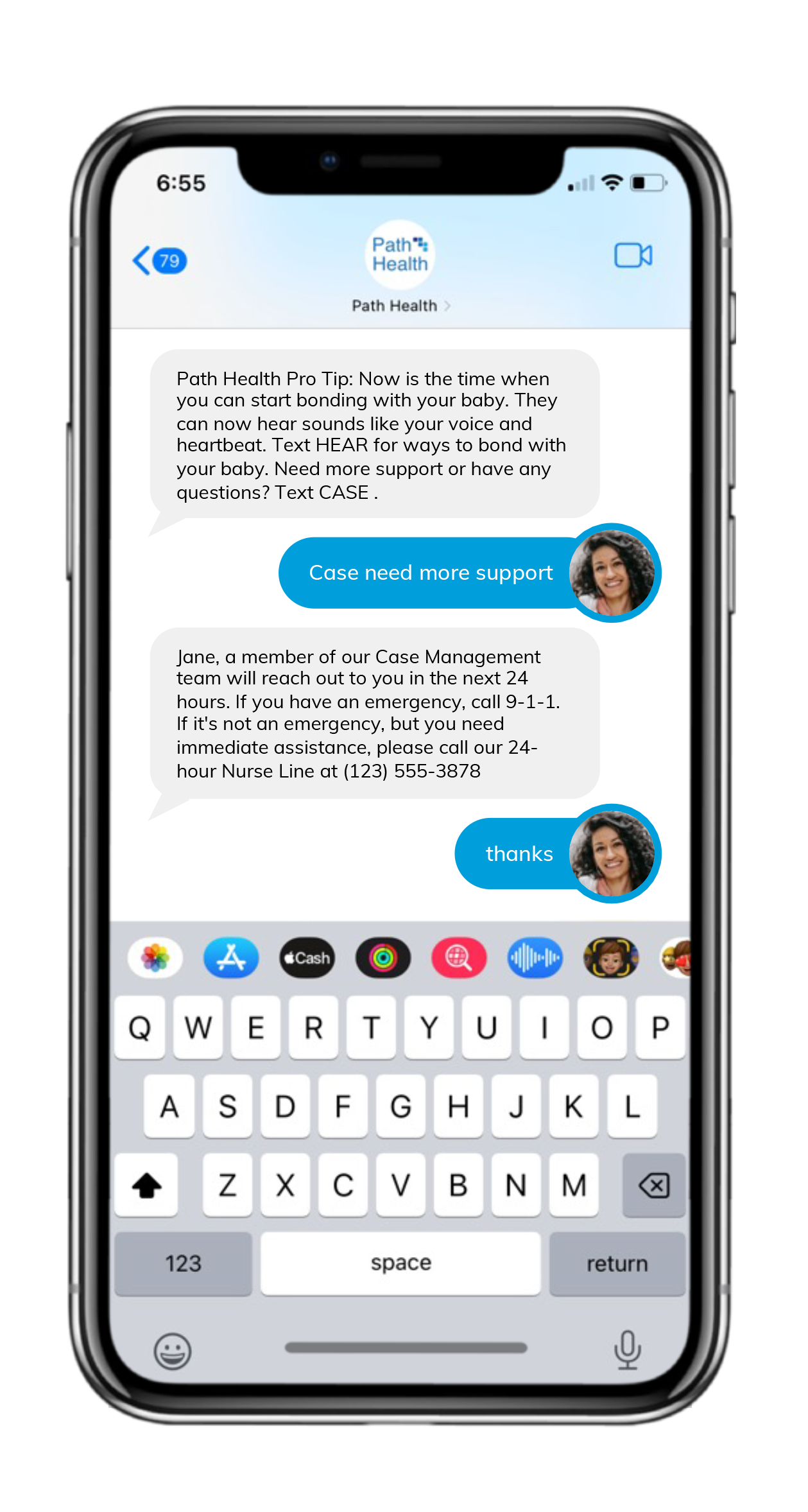
 The fotonovelas were created to address barriers such as procrastination, lack of self-care, lack of time, embarrassment about the process, and fear of results. They were developed in Spanish and English, in collaboration with the AltaMed Institute for Health Equity, and there were separate versions for men and women.
The fotonovelas were created to address barriers such as procrastination, lack of self-care, lack of time, embarrassment about the process, and fear of results. They were developed in Spanish and English, in collaboration with the AltaMed Institute for Health Equity, and there were separate versions for men and women.