Earlier this month, four of mPulse Mobile’s best and brightest subject matter experts packed up and headed to sunny Florida to attend The Strategic Solution Network’s (SSN) 14th Annual Medicaid Innovations Forum. A huge topic of conversation was, not surprisingly, the FCC’s Declaratory Ruling on phone outreach for redetermination. Released in late January, this ruling opened the door for plans to utilize texting in their efforts to maintain coverage for millions of Medicaid members.
Texting, however, has always been a big topic of conversation for us. 97% of US adults own a cell phone, and it seems everywhere you go people are glued to their devices. That is what makes SMS texting such an incredibly effective tool to add into your mix of channels. We spoke about just that during our session at the conference.
Healthcare Experiences Powered by Technology
For that session, Reva Sheehan, mPulse Mobile’s Senior Director of Customer Insights, had the opportunity to present onstage with Sammie Turner, Quality HEDIS Manager for Maryland Physician’s Care. Maryland Physicians Care, a customer of mPulse Mobile and the third largest Managed Care Organization in the state of Maryland, administers healthcare services to Maryland’s HealthChoice enrollees.
Maryland Physicians Care and mPulse partnered together to deploy a two-way SMS text campaign targeting multiple preventative care screenings, including Breast Cancer Screenings, Well-Child Visits, SSI, and Lead Screening in Children, and we delivered the results of that program to the audience.
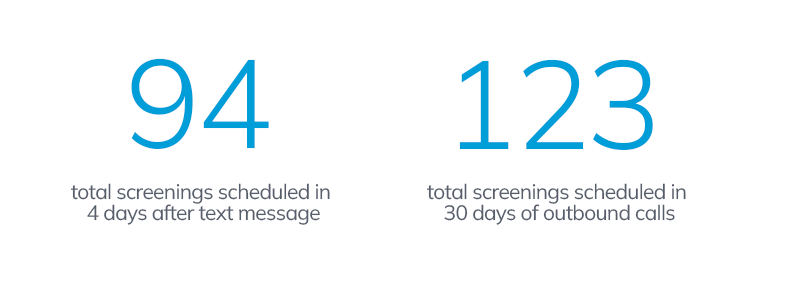
With reach rates ranging from 83% to 95%, we were able to target and communicate with thousands of their customers. The main metric we wanted to observe, however, was the success of texting compared to outbound calls. Is texting a more effective method of outreach to obtain scheduled appointments?
We focused on breast cancer screenings and found strong evidence that it was. After 30 days of outbound calls, 123 breast cancer screenings were scheduled. But with the texting program, we found that we were able to schedule 94 screenings in just four days.
The texting program was able to get 76% of the screenings scheduled that outbound calling did in just a fraction of the amount of time and did so without the manual work of call center representatives.
But why is this so? How is texting, which may seem less personal, able to have so much success so quickly?
Three Core Capabilities for Texting Outreach
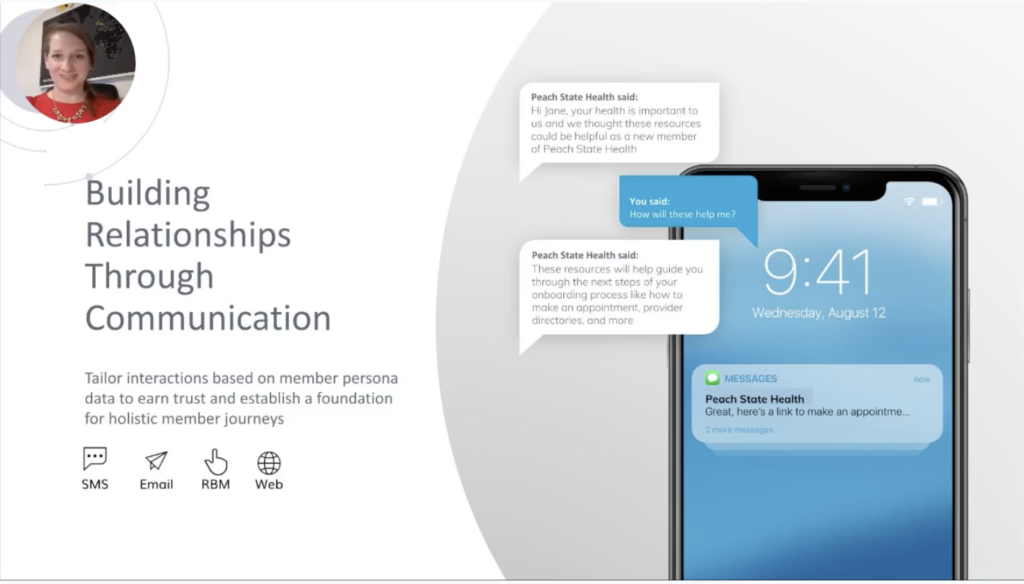
Texting allows us to reach a large population in a single event and assists in reducing the volume of outbound calls and or letters. If you have the right technology powering your texting program, however, it turns into more than just a text but into a dynamic two-way conversation that can be used to connect with a member, break down barriers to healthcare, and deliver better outcomes.
There are three core components that enabled this experience for Maryland Physicians Care’s members: two-way text capabilities, natural language understanding, and educational content.
Two-way Conversations Identify and Address Barriers to Care
When you have dynamic, interactive conversations with your members, you truly address the barriers they face when trying to get care. Lack of transportation, inability to get time off work, cost, and other factors all play a role in creating an inequitable health experience.
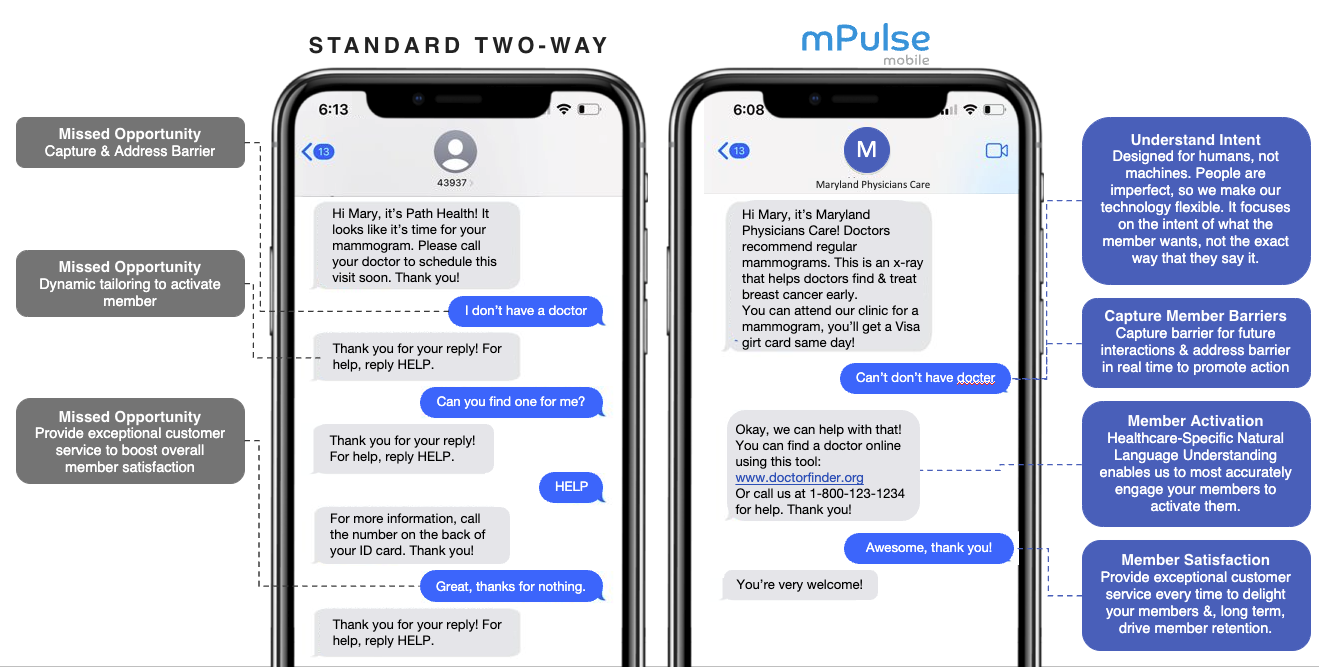
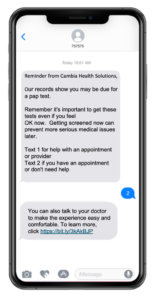
When a plan has the technology to have a real conversation with its members at scale, it can not only identify the reasons members aren’t scheduling screenings, but it can take it a step further to provide solutions and education for the member, such as helping them find a doctor like you see in the example below from Maryland Physicians Care’s program. When the door for care is opened a bit wider for one person, it makes the healthcare system a little bit more equitable for all.
Natural Language Understanding and Culturally Appropriate Content

Natural Language Understanding (NLU), a type of artificial intelligence, is the ability for our system to interpret the responses from the member (even if they are non-standard responses or slang) and respond back in an intelligent manner. mPule Mobile’s NLU is available in 7 languages with translation services for 13.
One example of NLU in Maryland Physicians Care’s program focuses on creating a more culturally sensitive experience. For this program, the two-way SMS content automatically converted from English to Spanish if the member responded in Spanish. Their language preferences were then reported back to the plan for future interactions. The ability to communicate with your health plan in the language that you are most comfortable with makes it much more likely that they’ll keep communicating and take the desired action.
Leveraging Educational Content to Promote Health Literacy
One thing we all know is how vital health literacy is to the concept of health equity. The ability to understand not only the care system, but your own body and healthcare needs is critical.
Videos can leverage educational content to help overcome barriers and inspire action by delivering bite-sized stories and entertainment straight to the member’s phone during a text exchange. The below example was used for a diabetes eye exam program run with a large national health plan. There was a 274% increase in link clicks to scheduling when this video was used in the text outreach vs when it wasn’t.
Equitable Healthcare for All
The dynamic conversational engagement used by Maryland Physicians Care enabled them to reach more members and deliver tailored resources and calls-to-action to empower members to act and deliver better outcomes at scale. When each member has the opportunity for a personalized and relevant conversation about their health with their plan, they’re receiving a more equitable experience.
Interested in these capabilities for a redetermination program? Learn how these same concepts can be applied to outreach around the end of continuous enrollment!