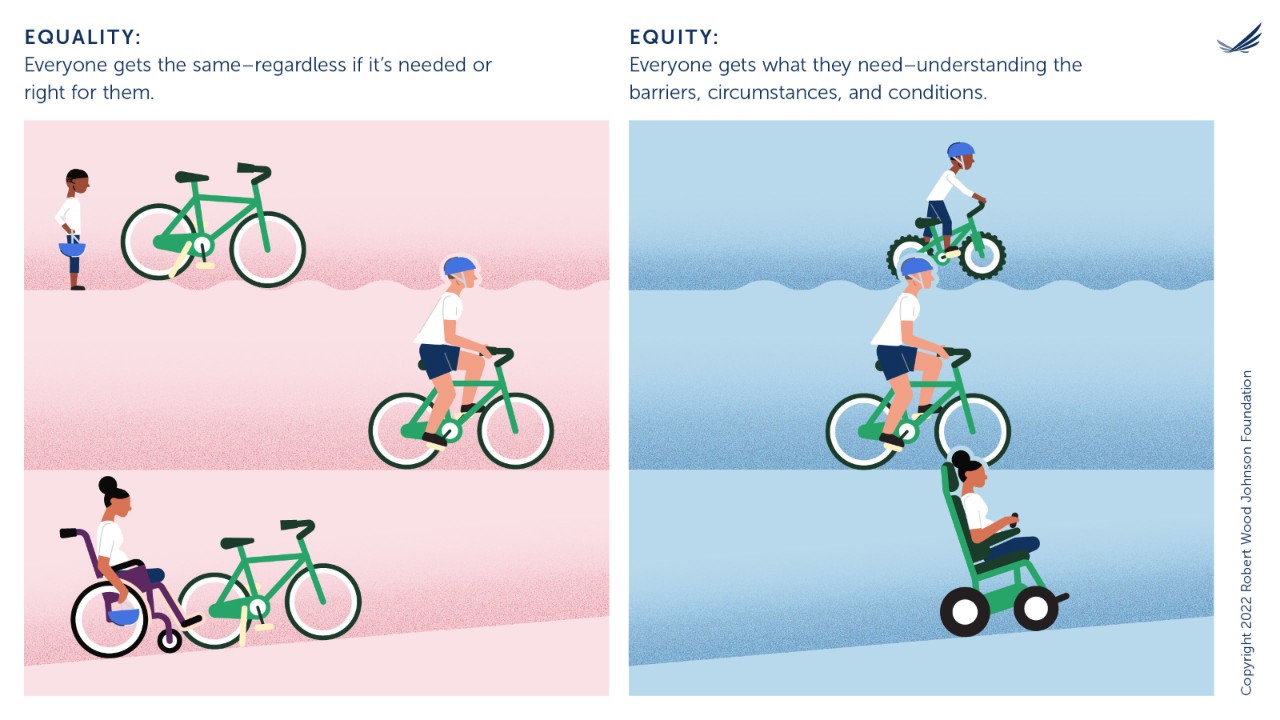
Patients are currently going through a transformation in the healthcare system. They are less like the patients we’ve always known them to be and are starting to act more like consumers. And what is the primary trait of a consumer? Choice.
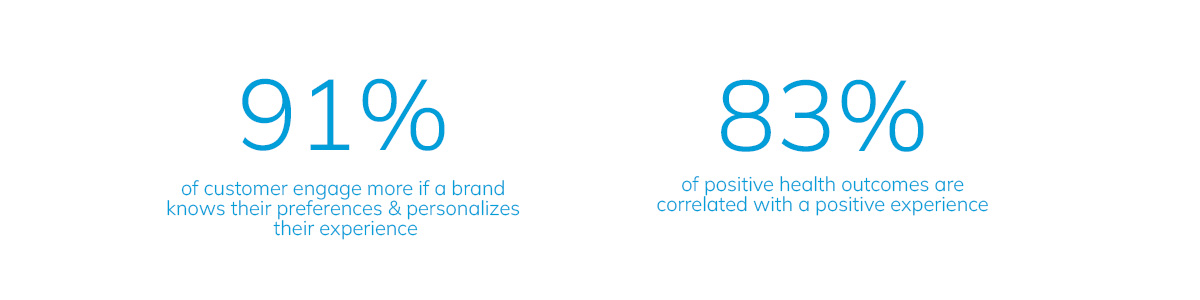
Patients today are fully fledged, active participants in their own healthcare and are making choices between different services and providers the way they make choices between brands. This changing dynamic requires that the healthcare system makes that shift right along with them. The goal of physicians, health systems, and accountable care organizations should be to ensure the patient’s experience is personalized, relevant, and on par with what they have come to expect from consumer experiences in all areas of their life. There are, however, some common challenges that we see healthcare organizations grappling with while moving toward this new normal, which can only be solved with the right mix of expertise and technology. But they can be solved for—with the result being a more valuable patient experience and relationship.
HealthCare is Challenging
It is. And these challenges are pervasive across many organizations we work with. We’re talking about gaps in Data, Technology Capabilities, Engagement Strategy, and Organizational Alignment.
Let’s dive into each one.
Data Gaps
Do you have the right cell phone number? Do you know if the number you have is even for a cell phone? Is it a land line instead? Do you have the correct contact preferences? Do you have information on their social determinants of health (SDoH) and the barriers to care they’re facing? This data can make all the difference when outreaching to patients and attempting to drive them to a specific action. How can you reach out to someone if you don’t have the right number? How can you affect someone’s behavior if you don’t understand their circumstances?
Solving for Data Gaps
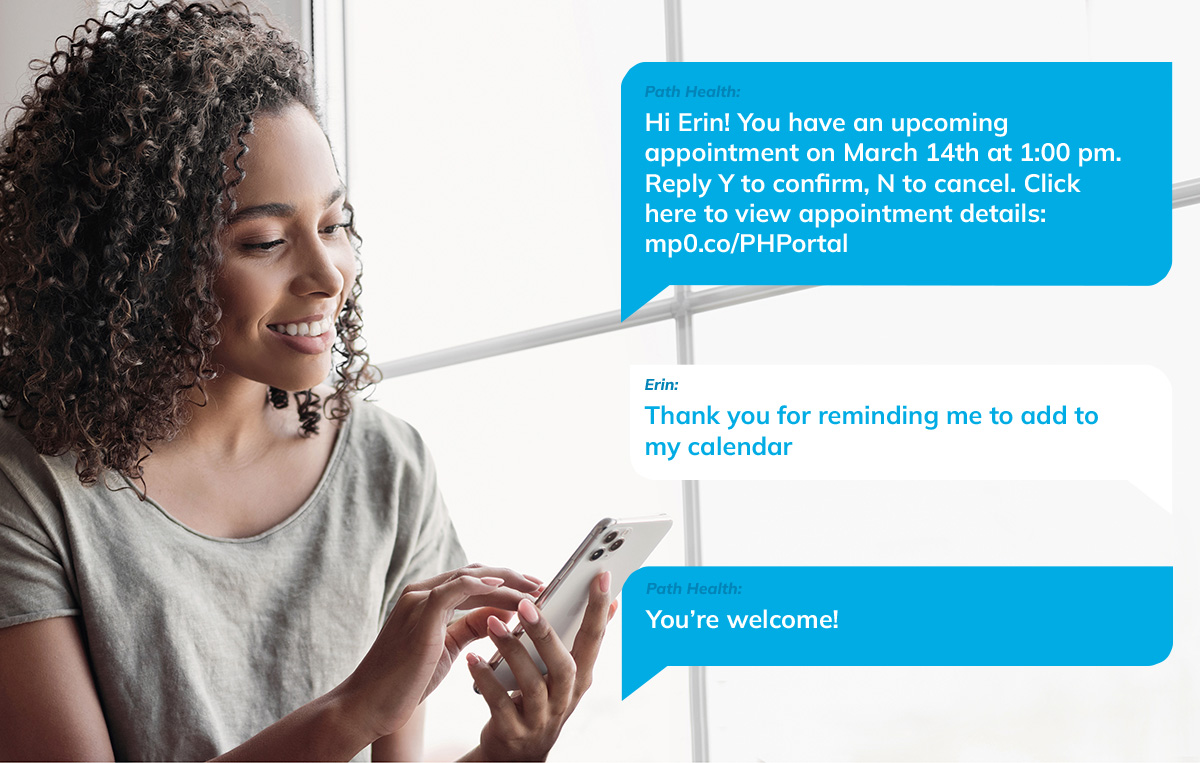
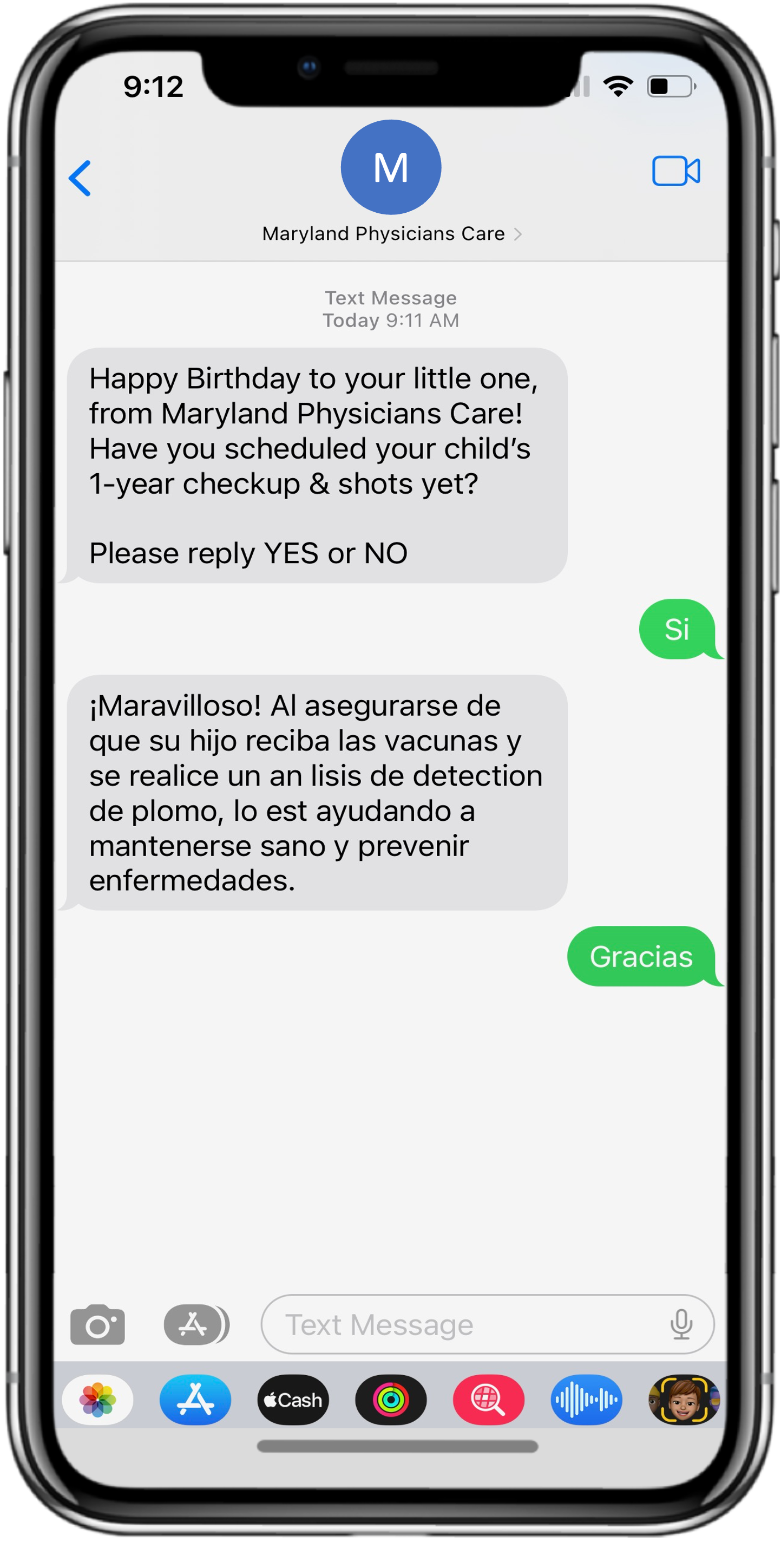
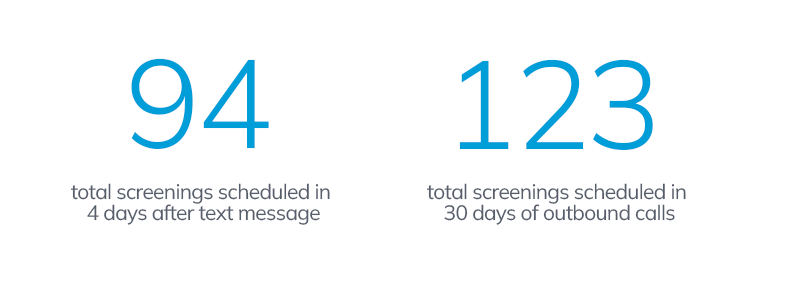
In all aspects of your outreach, you need to be data driven. This starts with the ability to collect and harness your data. An SDoH Index like mPulse Mobile has is the kind of data that allows you to tailor conversations to a person’s circumstances. Specific capabilities, such as two-way automated conversations, allows us to understand what people are doing and why they’re doing it. By being able to ask people directly and receive an answer, we can take that information, record it as data, and do analysis on it to identify trends. The most valuable insights you can have will come directly from your patients themselves. Of course, this can only be done at scale with the right technology.
Technology Capability Gaps
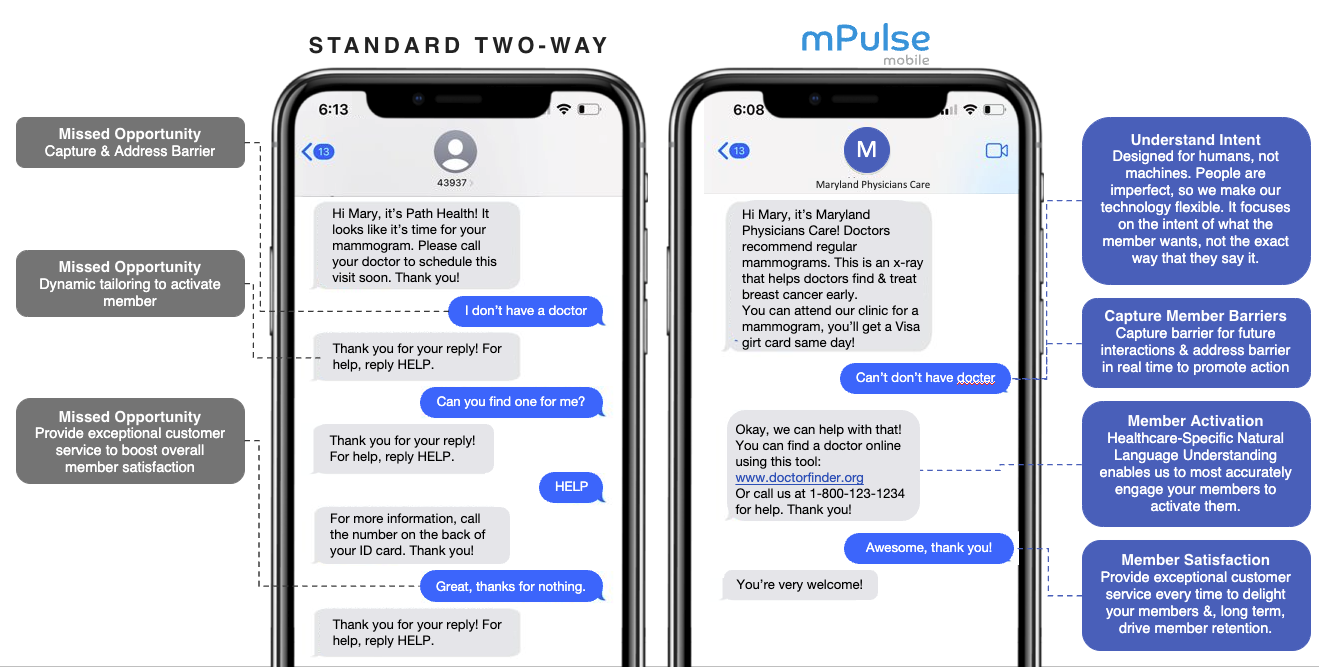
Having all the data in the world is little help if you don’t have the technology to use it at scale. You might be deploying one way messaging programs, which means you aren’t collecting information back from your patients to help personalize the conversation and further improve your interactions with them—and forget trying to do this on a 1:1 basis without the ability for your technology to automate these conversations.
Solving for Technology Capability Gaps
Conversational AI and Natural Language Understanding are two important foundational capabilities that can help close this gap. Conversational AI ensures you can tailor your conversation to the individual you’re speaking with, making it more likely you’ll connect with them and drive the desired action. With National language understanding, we can communicate with patients in a way that feels familiar, conversational, and natural. You get at the intent of what your patient is saying and account for humanness (such as typos or slang). At mPulse, we have linguists and computer programmers on staff who work together to come up with scripting that can interpret different combinations of languages, typos, and slang to get to the intention.
Gaps in Engagement Strategy
Maybe you do have the means to connect with your patients with two-way automated conversations. But are you saying the right things? Are your engagements tailored and optimized to ensure maximum outcomes? How often are you messaging? What’s the tone? Do you have a team dedicated to refining all these different aspects of your strategy?
Solving for Gaps in Engagement Strategy
When you understand how people think and make decisions, you can craft your outreach in a way that predicts their response and uses that prediction to nudge them in the direction you’d like. This is the reasoning behind the behavioral science techniques we bake into our solutions. Humans are fairly predictable, and we mostly react the same. Let’s use that predictability to push them toward healthy behaviors! Many behavioral science techniques are used to build our programs: cognitive overload could determine the pacing of our program; authority bias may dictate who we have giving the information; and storytelling effect could dictations how we give the information;
Gaps in Organizational Alignment
Your patient has gotten your messaging, they’ve made the appointment. Now, are you guiding them through transition of care in the most effective way possible? For example, ensuring they’re scheduling an appointment with a PCP after an ER visit.
Solving for Gaps in Organizational Alignment
The goal is to produce trust-building patient experiences consistent across the entire experience with a brand. For this, we have enterprise engagement, which allows us to handle the scale necessary for organizations which can have 100,000+ patients.
We need experiences consistent across that member base while also personalized to match each individual’s needs. That’s a tall order. And this comes back full circle to data and technology—both are needed to ensure this patient experience is protected.
The New Normal
Digital trends are changing the game. Patient expectations are changing the game. The choices they have and the experiences in everyday life they’ve grown used to are creating new rules of the road in healthcare. As it should. We have technology in the market today that allows these experiences to be exceptional, so why should they (and we) settle for anything less?