912 days sit between the beginning of the Public Health Emergency (PHE) and today, July 26, 2022. The PHE has been renewed 10 times, with the latest extension set to expire on October 13, 2022. There has been no shortage of speculation around the last two extensions, especially after the Biden-Harris administration committed to providing states with at least a 60 day notice prior to its plans to terminate or allow the PHE to end.
In March of 2020, the Families First Coronavirus Response Act (FFCRA) was signed into law. This particular piece of legislation focused on many programs impacting children and families, including but not limited to Supplemental Nutritional Assistance Program (SNAP), the Women Infants and Children (WIC) program, family and medical leave, school lunch, emergency paid sick leave, and state based programs for Medicaid and Children’s Health Insurance Program (CHIP) eligibility and enrollment requirements. The latter of these provisions effectively froze Medicaid disenrollment during the PHE allowing for continuous coverage for current beneficiaries. Prior to the pandemic, states were required to reprocess eligibility for most of its enrollees on an annual basis, this process is referred to as redetermination.
Medicaid and CHIP enrollments have increased by approximately 19% or 13.6 million enrollees between February 2020 and September 2021 with an additional 1.2 million enrollees added to the roster since the September report. To offset increased program spending coupled with decreased state tax revenue, the FFCRA authorized a 6.2 percentage point increase in the Federal Medical Assistance Program (FMAP) and in return expected continuous enrollment. This FMAP bump will continue through the end of the first quarter in which the PHE ends.
When the End Comes…
Now that we’ve covered some of the basics, let’s look what it means for the plan when the PHE and continuous enrollment ends, and redetermination resumes for its beneficiaries. The end of continuous enrollment is expected to create the single largest health coverage transition since the first Marketplace Open Enrollment. Due to the high volume of unprocessed eligibility renewals and the increase in membership, states have been given a 12-month unwinding period to manage this administrative task. The Department of Health and Human Services (HHS) has issued an Unwinding Toolkit and CMS has encouraged states to only process 1/9 of its total caseload in a single month; processing more than this creates an increased risk of people falling through the cracks and being unnecessarily disenrolled resulting in a loss of coverage and potential increase of additional administrative work to bring them back in.
Keep in mind each state will have its own pathway and plan to work through this transitional phase. For example, some states have indicated they will target enrollees who appear to no longer be eligible first and others plan to conduct renewals on a monthly basis based on the individual’s initial enrollment month and some states have also reported they plan to process the backlog as soon as 3-6 months with others using the full 12 plus months.
Projections for total Medicaid and CHIP growth during the pandemic and scenarios calculating total loss of coverage continue to shift and grow with varying levels of certainty and range from 5 to 14 million enrollees losing coverage. Even at the lowest end of the loss projections, five million people is an awful lot! While some loss may not be preventable, complete, and total disruption can be avoidable for those who be eligible for coverage on a Marketplace (aka Affordable Care Act or ACA) plan. This shift to retention will be more bearable and less burdensome if American Rescue Plan Act (ARPA) subsidies continue for the estimated 13 million Marketplace enrollees currently receiving a premium reducing subsidy.
Planning for the Unwinding of Continuous Enrollment
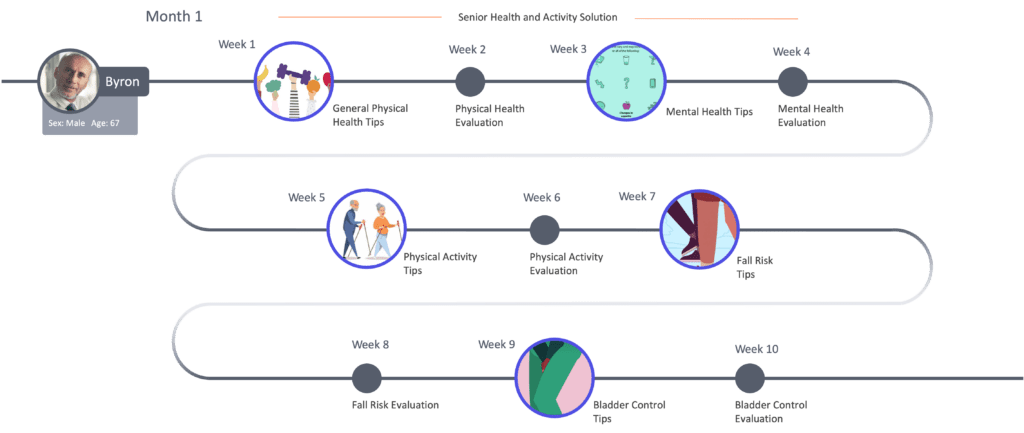
So, we’ve covered some basics on what it means for the plan (a lot of work ahead), what it means for the member (a lot of uncertainty still remains), and now about what it means to everyone in between which in this instance is us, mPulse and that’s where I start to get excited. There are phased approaches and best practices from our friends in California who have been given the green light to reach members in just about any way possible even allowing plans to solicit opt-in consent for future updates by text message to the East coast where communications to CoverVA enrollees in Virginia are being encouraged to update their contact information by signing up for email or text alerts and following via social media.
I’m no math whiz, but this one is easy: X + 14 = Regular Redetermination Resumes
With X being the unknown number of additional PHE extensions and 14 the number of total months allowed to manage the backlog at the end of the PHE you’ll find yourself back where you were before COVID-19 was a household name. Regardless of where you are in your own state’s phase approach, you can count on trusted partners like mPulse to engage the unengaged and reach the unreachable in your membership. Not sure where to start? Reach out to learn more about the power of SMS and find out how many of your contact numbers are mobile vs. land lines.