Have you ever wondered why Amazon provides its recommendations or why Netflix tailors your movie menu? It’s not because they must, dear readers. It’s because they know the power of behavioral science.
They both have behavioral science and psychology marketing teams working on the user experience and are uniquely aware of the constant barrage of advertisements and marketing that their consumers are being hit with throughout the day. People, including members we are trying to reach, see between 4k and 10k ads and make about 35,000 decisions every day. To complicate things further, 87% of information is subconsciously filtered. So, most of the time it can be next to impossible to get through to members.
So, you might be asking yourself what is behavioral science? And why does it matter for health communication?
Behavioral science describes the study of behavior through experimentation and observation. Behavioral scientists’ study when and why individuals engage in specific behaviors by examining the impact of factors such as conscious thoughts, motivation, social influences, contextual effects, and habits.
Behavioral science research is diverse and expansive. There is an abundance of work showing that human reasoning does not conform to what common sense predicts. Behavioral scientists study why people sometimes behave in a way that may not maximize their own well-being, such as making choices in the present that do not maximize their happiness in the future; examining how seemingly arbitrary contextual factors influence our decisions, beliefs, and attitudes or test how different incentives affect people’s motivation and behavior.
Learn more about using behavioral science in health communications by viewing our on-demand webinar, Frictionless Healthcare: Fueling Behavior Change »
So, readers, you might be asking yourself how do you apply these ideas in healthcare or health behavior change? If we really want to drive behavior change, we need to understand how people behave. When it comes down to it, there’s a lot of human behavior that we can explain in terms of two simple forces: Friction and Fuel. A rocket ship is a helpful metaphor that Dan Ariely uses to describe behavior change. To get a rocket ship moving, you need to increase fuel and decrease friction. To change behavior, you need to increase fuel (increasing motivation) and decrease friction (removing barriers). And it turns out, these concepts play out quite well in healthcare, so let’s examine that.
The Friction
In healthcare, frictions are anything that get in the way of your member performing a positive health behavior. Friction is typically caused by uncertainty on the part of your member. They could be uncertain about how hard an action will be, how long it will take, or how much it will cost.
Technology can go a long way to uncover and decrease friction.
One way is to employ barrier messages to uncover challenges (the friction) a member may be facing. Barrier messages are specific questions posed based on research of top barriers for specific audiences with specific health actions. Barriers happen. Why not proactively create opportunities to uncover and address them?
Once the barrier is discovered, we can work to solve it then drive motivation using proven behavior science techniques. You can see examples of those barrier messages below and observe how in a short phone screen you can do a lot to try to reduce barriers and increase motivation.
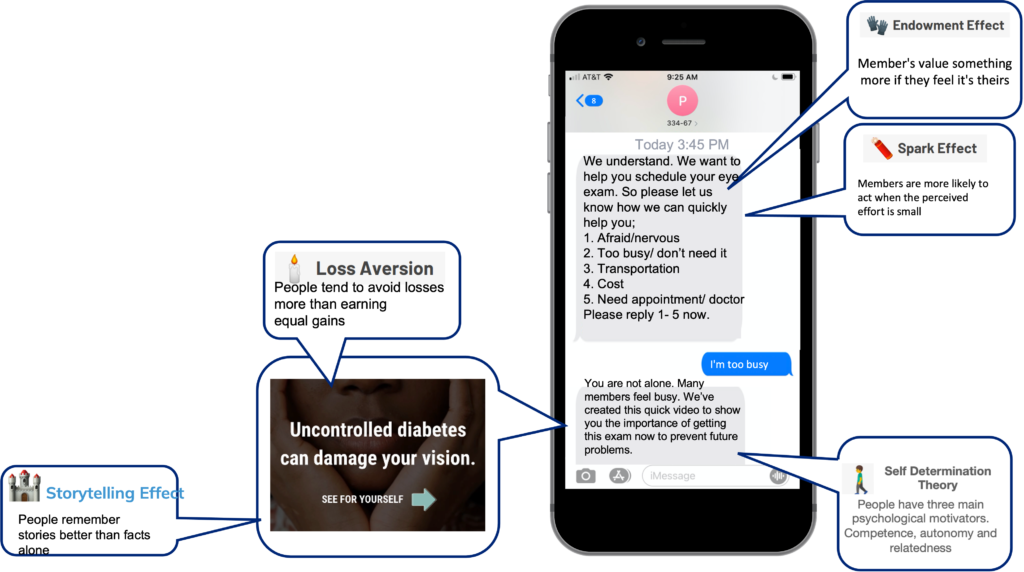
The Fuel
Speaking of motivation, fuel is anything that makes a positive health behavior more appealing . This could be member testimonials that utilize people copy the actions of others in an attempt to undertake behavior in a given situation) or an offering using incentives to activate the concept of reciprocity. Or you could utilize the endowment effect in messaging (an emotional bias that causes individuals to value an owned object higher, often irrationally, than its market value) like The Behavior Change for Good Initiative (BCFG) did to boost flu vaccine rates by up to 11%. The most powerful of these vaccination texts simply used ‘reserved for you’ messaging.
. This could be member testimonials that utilize people copy the actions of others in an attempt to undertake behavior in a given situation) or an offering using incentives to activate the concept of reciprocity. Or you could utilize the endowment effect in messaging (an emotional bias that causes individuals to value an owned object higher, often irrationally, than its market value) like The Behavior Change for Good Initiative (BCFG) did to boost flu vaccine rates by up to 11%. The most powerful of these vaccination texts simply used ‘reserved for you’ messaging.
One of the ways we use these concepts is in stories or fotonovelas. This format is something members are used to seeing on social media, are they are quick and viewable on-the-go.
The Big Picture
Behavioral science can be tricky, but you can use the concept of friction and fuel to make a big difference in behavior change. This post was just an introduction to friction and fuel in healthcare, but we’ll be following up with a lot more information around the specific concepts and examples of each, so stay tuned for part 2!