To say the events of the last year had an unprecedented and unconventional impact on health plans would be an understatement. From early January 2020 when Health and Human Services (HHS) declared a Public Health Emergency (PHE) to aid the nation’s healthcare systems in responding to COVID-19 through the cancellation of the 2020 HEDIS and CAHPS collection and now with vaccines becoming vaccinations, the Centers for Medicare and Medicaid Services (CMS) has worked tirelessly to continue its pledge to put patients first in all programs.
To put patients first in all programs, you have to address their needs and provide support to the plans, practitioners, and communities who care for our most vulnerable populations. With the earlier than anticipated release of the 2022 Medicare Advantage and Part D Advance Notice Part II, CMS provided plan sponsors more time to prepare their bids during unprecedented times. While the better part of this Advance Notice focused on rate and payment policy, it provided plans with important updates and changes related to the Star Rating program which can have a tremendous impact on Quality Bonus Payments (QBP).
Following the earlier-than-anticipated Advance Notice in October 2020 came the equally early Final Rule in January 2021. Here are a few noteworthy changes that we discussed in the fall that are here to stay for 2022. For a deeper discussion, watch the 2021 Star Ratings panel with Rex Wallace, Jim Burke, and myself below.
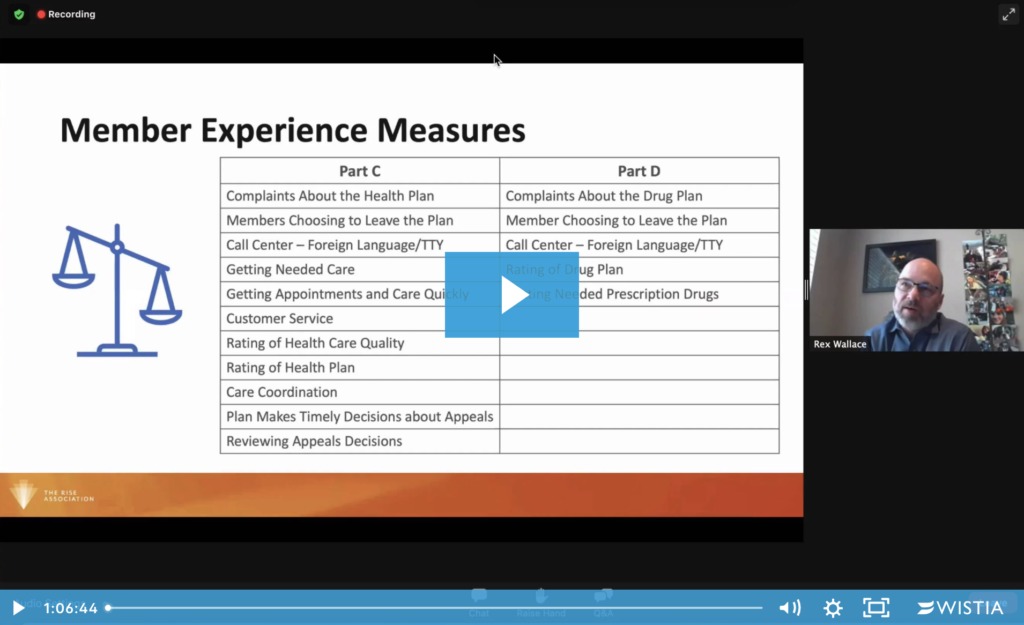
- CAHPS and the Member Experience. CMS is making good on its promise to lend a bigger voice to the beneficiary and will proceed with the increased weight of its member experience measures, including the Consumer Assessment of Health Plans and Systems aka CAHPS survey. While the 2021 CAHPS survey will still have a weight of 2x each (not including the flu measure) for the 2022 Star Ratings, the importance of member experience and perception is greater than ever as these measures will contribute to over 50% of the overall weight in 2023 Stars. Even the best and most robust regulatory and off-cycle surveys will only represent a small percentage of members at one moment in time. Plans need more experiential and real time data around common and frequently used benefits that scales not only the entire member population, but the entire member year. mPulse Mobile has developed an event-based check-in program that not only gathers valuable member experience and sentiment data, but also has the ability to address dissatisfaction and solve common pain points in real time using its patented natural language understanding and conversational messaging. Learn more about our CAHPS Solution.
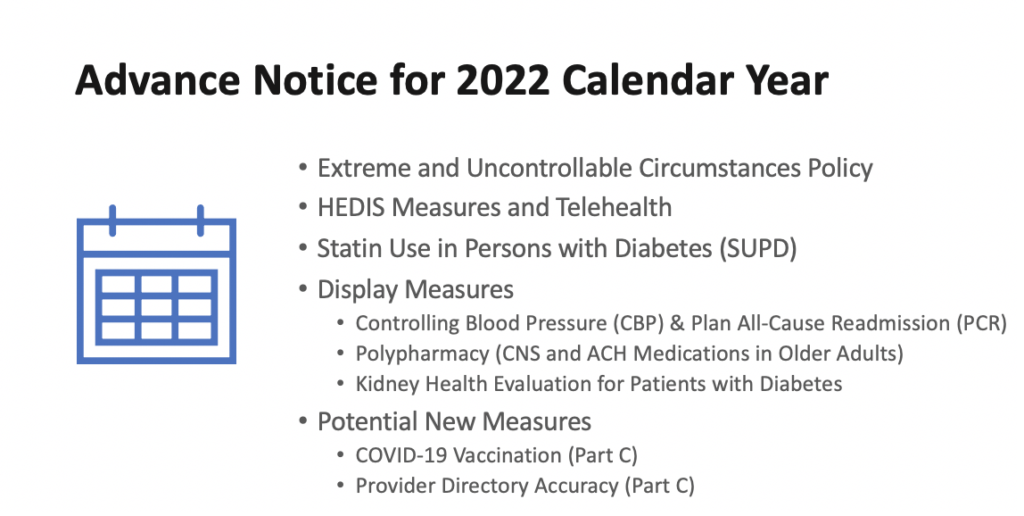
- Extreme and Uncontrollable Circumstances Policy was amended to note any additional COVID-19 relief under this policy for 2021 measurement year will have to come through future rule making. CMS adjusted its disaster policy and plans will be allowed to use the ‘better of’ between some of its 2021 and 2022 measure ratings. This ‘better of’ method may produce inflated performance numbers that will be difficult to sustain in future years. Plans should proactively identify their at risk areas and deploy a strategy at scale to offset a potential loss in QBP for future years.
- With no new measures for 2022 and some remaining on the display for another year, plans will have the opportunity to continue efforts to close gaps, connect members to appropriate care, and review their data for one more year. Controlling Blood Pressure and Plan All Cause Readmissions will remain on display and likely return to the active page with a 1x weight for their first respective years. The potential introduction of a COVID-19 measure did not receive positive feedback during the open comment period and only time will tell if it was related to the reluctancy of accepting COVID-19 isn’t really going away anytime soon or the proposed collection and impact another vaccine measure may have on Stars.
- HEDIS and Telehealth is here to stay and work together. According to the American Journal of Managed Care, telehealth claim lines increased 3.060 percent nationally from October 2019 to October 2020. As members seek care outside of the traditional office setting, providers and payers still have a need and obligation to capture the full burden of illness and these updates include additional code sets to be allowed for measure inclusion or exclusion when captured via telehealth visits alone. This is just another example of how members, plans, and providers are embracing digital technologies.
- Part D measures, above all other measures for 2021 Star Ratings, got harder. Sure, some may think this could be attributed to CMS not having any CAHPS or HEDIS measures to use in their methodology calculations, but the increase in cut points should be attributed to an increase in performance across all of the eligible plans. Barriers to proper medication use and adherence are much greater than cost and access, especially as plans increased mail order access during the height of COVID-19. We often see poorer adherence and participation from members with the lowest cost share which tells us that what they really need is increased education and engagement. Simple one-way refill reminders for your adherence measures or offers to complete a Comprehensive Medication Review (CMR) for your Medication Therapy Management (MTM) program are no longer enough to compete with those top performing plans who are driving those cut-points higher every year. Learn more about our Medication Adherence Solution.
As shots go into arms and some semblance of normalcy begins to return, it’s still too soon to know the full impact the pandemic will have on members, plans, providers, technologies and so much more. CMS has equipped plans with a sneak peek of what’s to come and extra time to prepare for it in an effort to take better care of its members. It’s never too late to develop or enhance your member engagement strategy. How will you continue to wrap your arms around your members throughout the year and beyond COVID-19?