We’re happy to announce our participation in the 2022 BCBS National Summit was a success! In early May, mPulse Mobile sent our strongest health engagement experts to The Orange State to attend and speak at the Summit, and they returned with valuable insights, new connections, and a reaffirmed belief in the power of health engagement designed for consumers.
Chris Nicholson, mPulse CEO, Magdalen Kmiec, Vice President of Engagement Strategy, Christian Bagge, National Account Executive, and Reva Sheehan, Director of Customer Insights, met and talked with leaders from many different Blues plans gathering stories from the front lines of healthcare and swapping viewpoints on the newest trends in healthcare engagement.
For us, the conference was a chance to meet with our current BCBS customers and have in-person discussions about their engagement programs and overall experiences with our platform. We also took the opportunity, however, to branch out and meet other BCBS leaders with whom we’ve not yet worked and have an exchange of information about our respective places in the healthcare space. These conversations gave us better insight into the landscape they’re navigating and confidence that the direction we’re taking for our customers is indeed the best course.
From Members to Consumers: Healthcare in the Digital Age
One reoccurring theme from our conversations at the summit was the age-old struggle to drive healthy action and meet requirements set by CMS, but many of these discussions showed the health industry could be looking at it all wrong. Magdalen Kmiec discussed this during our joint presentation with Aimee Viles, Vice President of Digital Solutions for Cambia Health, Scaled for Many, Tailored to One: Leveraging Data to Impact Member Engagement.
Her main message was that members are no longer just members. Our members live in an Amazon and Netflix world where their needs are anticipated and delivered on before they can even ask. Their digital and real world lives are now seamless and fluid. And they don’t shed these experiences and customer service expectations when they interact with their health plans.
Yet the healthcare industry has not created that same experience for their health consumers – but they can. That’s where Magdalen overviewed the four essential pillars of engagement: rich customer data, channel optimization, empowering content, and robust behavioral science.
Rich Customer Data
Plans have rich data on file, but are they using it? From the results of the member’s most recent A1c test to the date of their last wellness exam, data can be harnessed to create a better experience.
Equally important, though, is to gain data through conversations with your members. Language preferences, sentiment toward the plan or program, social determinants of health (SDoH) factors, and more are valuable data points that can be added to the file for each member. Then your future conversations will become much more tailored.
Channel Optimization
Customer expectations are evolving rapidly, and our health consumers expect consistent, accurate, and timely information at their fingertips regardless of the channel they see it. Omnichannel is no longer a nice-to-have but a necessity to remain competitive.
The trick is to eliminate the silos between your channels and have them work together in a way that creates a single experience. So IVR, social media, SMS messaging, and streaming health content – it’s all working in sync to tell the same story.
Empowering Content
Low health literacy is a main driver of inaction. By delivering tailored, bite-sized streaming content in the moment based off insights gathered during conversational outreach, you are immediately addressing barriers and educating at the same time. Whether it by interactive stories, animations, or mini lessons to full courses, it gives the plan a chance to engage and empower in a more impactful way than can just be done by text message.
Robust Behavioral Science
There are two main questions for behavior change: Why would people want to do the behavior? Why aren’t they doing it already?
The ability to harness behavioral science , which tells us how people are likely to react and why, enables you to answer these questions and then leverage that information to drive behavior change. Put simply, people are irrational in predictable ways, so use that predicable irrationality to steer them in the direction of healthy behaviors. It’s the same methods used by companies like Amazon, Walmart, Target, and many other big major corporations – and it works.
Cambia Health: Gaps in Care and Rx Refill Program Outcomes
Cambia Health, our co-presenter at the summit and current client, is an ideal example of the members to consumers concept being effectively utilized, so Aimee joined Magdalen onstage to present two programs Cambia Health ran in partnership with mPulse Mobile.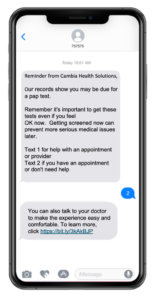
The first was aimed at closing gaps in care for Cervical, Breast, and Colon Cancer screenings. Built on a foundation of behavioral science, the program outreached to 106,433 members across Commercial HCA, Commercial Non-HCA, Marketplace, and Medicare Advantage gather opt-in consent through SMS messaging (response required) before commencing.
Based on member reporting through this program, it was discovered the top 3 insights into why they weren’t completing the screening were:
- they already completing the screening
- they were too busy
- they thought the screenings were unnecessary
This is valuable information for a plan to have because it gives data with which to communicate further. For example, for those health consumers who think screenings are unnecessary, the plan could send streaming health content explaining the importance of the screening their missing (such as the breast cancer screening lesson you see below). And for those who already completed, the plan can use two-way SMS to collect more info on when or where that screening took place and amend their records.
The second program Aimee presented was an Rx Refill Engagement program with a 4-star goal for Part D medication adherence measures. This program included 48,980 MA members with active opt in and it was design as an interactive SMS program with conversational tailoring, follow up reminders, and barrier assessment. Refill rates with the solution were 85%, there was 72% positive feedback, and 20% of members requested additional reminders.
Looking Forward to More
We enjoyed the chance to join and network with all the Blues plans to discuss the future of healthcare engagement and how technology can play a huge role in it, and we can’t wait to return next year!