On October 29, 2021, the FDA authorized usage of the Pfizer-BioNTech COVID-19 vaccine for children ages 5 to 11-years-old. This was followed by the CDC’s announcement four days later recommending the pediatric COVID-19 vaccine for the 5 to 11 age group. Now that 28 million more Americans are eligible to receive the vaccine, healthcare organizations must play an important role accelerating vaccinations and decreasing the spread of the virus.
Routine child immunizations have declined over the last few years and have continued to drop since the emergence of a new virus. Recent data from the World Health Organization (WHO) indicates that in 2020, over 23 million children missed out on basic vaccinations, which is 3.7 million more than in 2019. Children make up a large segment of the U.S. population and can substantially advance the spread of COVID-19, elevating the need to promote vaccine awareness to parents of eligible children.
To increase vaccination among 5 to 11-year-olds, it’s important to first understand what causes vaccine hesitancy in parents. Social determinants of health (SDOH), misinformation, and health access are a few factors that influence vaccine hesitancy, and healthcare organizations can overcome obstacles like these by incorporating behavioral science strategies when communicating with parents. Overcoming vaccine barriers requires that parents are engaged with the appropriate educational resources that inspire behavior change and promote self-efficacy.
Understanding the Importance of Vaccinating 5 to 11-year-old Children
In the United States, there are over 72 million children under the age of 18, accounting for roughly 22% of the total population, according to a recent report from the U.S. Census Bureau. While the 12 to 17-year-old population is 51% fully vaccinated, those numbers are declining. The addition of 5 to 11-year-olds into the population of eligible Americans means that 28 million new patients are now able to be vaccinated. The data suggests that there are over 40 million children yet to be vaccinated, and well over half of them are between 5 and 11-years-old.
The urgency with vaccinating these children lies in the threat of widespread COVID-19 infection. 5 to 11-year-old children represent a large portion of the population across the U.S., and more importantly, they can infect vulnerable groups around them unknowingly through asymptomatic spread. Additionally, as the virus spreads throughout the community, the emergence of a more contagious COVID variant becomes increasingly likely. This complicates the pandemic by not only by bringing this unknown factor into the equation but by also potentially threatening the efficacy of existing vaccines for the greater population.
Beyond the threat of the coronavirus itself, however, required social isolation has contributed to loneliness and anxiety in children. The National Institute for Health Care Management Foundation (NIHCM) reported that from mid-March 2020 to October 2020, mental health-related Emergency Department Visits for children ages 5 to 11 had increased 24% compared to the previous year. Returning to a normal, pre-pandemic lifestyle may be critical to protect the long-term mental health of children.
So, if vaccinating the youngest eligible population is a step in the direction of normalcy, what is stopping parents from acting?
Identifying Barriers That Cause Vaccine Hesitancy
Perhaps the most apparent obstacles in the way of widespread vaccination among 5 to 11-year-old children are the education level, healthcare access, and health beliefs of the parents. In a study from Northwestern University that surveyed over 1,900 parents, it was found that those who received less education were less likely to vaccinate their kids. Fortunately, insights from older populations demonstrate that personal health beliefs and misinformation can be mitigated by providing adults with accurate COVID-19 information from trusted health experts and trusted channels of communication.
Lack of healthcare access can prevent parents from receiving vital communication about the free cost of the vaccine, locating vaccination sites, or how safe the vaccination itself can be (91% effective in preventing COVID-19 in children ages 5-11 years-old). Those populations with lower incomes are less likely to have healthcare coverage, which ultimately negatively influences vaccination rates.
When evaluating low access to COVID-19 resources, understanding how race and SDOH influence program utilization can help illuminate the best strategies to reach a parent. The aforementioned study also found that when it comes to vaccinating their children, Black American parents were the most hesitant racial group. This presents an opportunity to deliver more personalized interactions that scale across diverse populations. In order to do that, it becomes necessary to engage parents with culturally sensitive and accurate vaccine information.
Each individual parent has unique beliefs and preferences that influence how they engage with a COVID-19 program. Barriers like misinformation, SDOH, and health access can significantly impact vaccine hesitancy. While these are ingrained beliefs and difficult obstacles to overcome, healthcare organizations can adopt strategies to uncover these barriers and inspire healthier actions through meaningful conversations tailored to each individual’s unique beliefs and barriers.
Overcoming Barriers with Behavioral Science
The barriers that create COVID-19 vaccine hesitancy in parents are similar to the barriers that have long existed with traditional immunizations like influenza. Just like with the flu, an individual’s preferences can be understood by incorporating behavioral science strategies like social proof, authority, perceived effort, and affect.
Social proof is a concept derived from the Self Determination Theory, which suggests people can be motivated by their psychological needs for autonomy, competence, and relatedness. Giving people social proof, such as stories from parents like themselves who have already vaccinated their own children, ensures parents that they are not alone.
Authority is the inclusion of trusted health experts to improve vaccine education and reduce misinformation. When vital information is shared through clear and convenient conversations, organizations can begin to build trust with parents and drive health literacy.
The idea of perceived effort stems from providing accessible resources like FAQs or vaccine finder. This concept inspires self-efficacy by empowering parents to learn more about COVID-19, making it easier to take action.
Finally, incorporating a concept like affect ensures that messaging to parents is based in empathy and compassion. Communication should exhibit sensitivity to ensure parents feel comfortable discussing their child’s healthcare.
By gathering data directly from parents through behavioral science, healthcare organizations can tailor conversations according to the parent’s preferred language and preferred channel of communication.
Tailoring Conversations and Content to Drive Vaccine Readiness
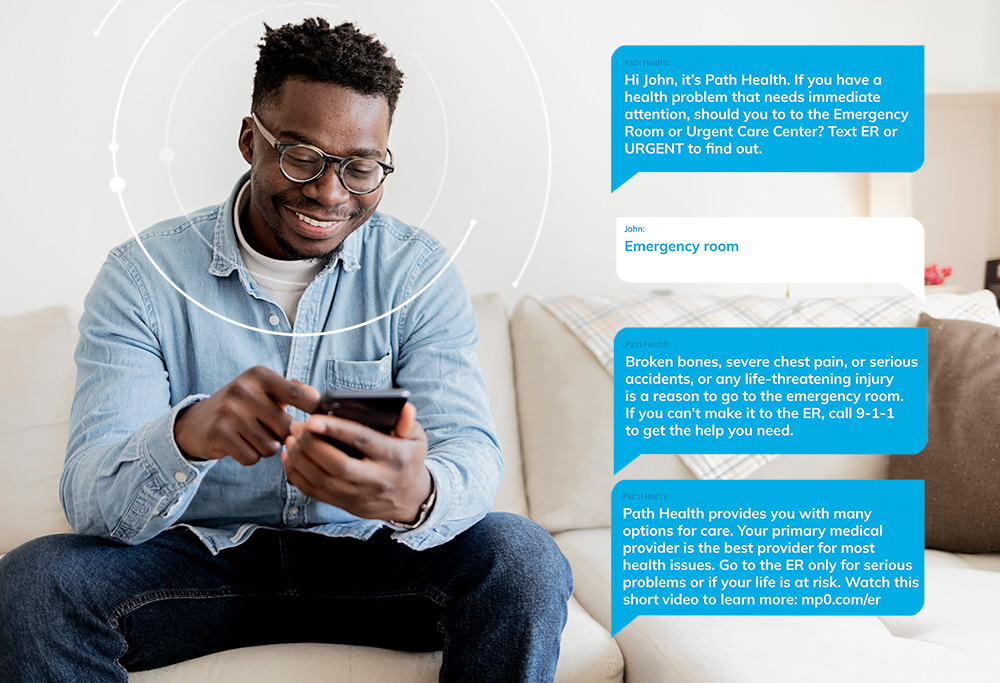
All the behavioral science theories above can be employed when building an effective vaccine engagement strategy. One way healthcare organizations have begun fighting vaccine hesitancy throughout the last year is by utilizing Conversational AI solutions and streaming health content to educate their populations.
Personalized interactions with parents offer insights into how to keep them engaged with a program. By leveraging Conversational AI solutions, organizations can scale the number of conversations they are having while ensuring messages are tailored to each recipient. When employing two-way dialogue, unique barriers can be tackled by providing appropriate health resources and information to challenge their beliefs. One health plan saw member response rates of 19% for a COVID-19 vaccine engagement program. The plan understood that certain healthcare consumers may not respond to traditional methods of communication, enabling new and innovative approaches to lift vaccine awareness and readiness.
Access more resources for COVID-19 vaccine engagement >>
 By providing streaming health education to parent populations, they can easily access a library of COVID-19 learning content from trusted health experts. The easily digestible nature of streaming educational videos and podcasts makes it easy for both parents and children to follow along. The adoption of tailored conversations and rich, learning content yields a 69% average completion rate of on-demand COVID-19 content.
By providing streaming health education to parent populations, they can easily access a library of COVID-19 learning content from trusted health experts. The easily digestible nature of streaming educational videos and podcasts makes it easy for both parents and children to follow along. The adoption of tailored conversations and rich, learning content yields a 69% average completion rate of on-demand COVID-19 content.
While engagement is necessary to improve vaccine education, providing a tailored learning experience is driving the most impressive outcomes related to program satisfaction. Personalization inspires program engagement that scales populations and is helping health plans achieve results like 70% member satisfaction. When healthcare organizations deploy educational COVID-19 video content, they encourage parents and children to learn more about the vaccine while positively impacting consumer experience.
Parents should be met with meaningful dialogue and content that is convenient to them. The use of behavioral science enables the understanding of parents’ personal beliefs and preferences, helping uncover barriers and information gaps. By incorporating tailored conversations and streaming content, healthcare organizations overcome those barriers, creating a seamless consumer experience that lifts health literacy and self-efficacy. Parents who are empowered with accurate health information and accessible resources can reduce vaccine hesitancy and significantly improve vaccine readiness for their children.